Article No. 378
22 September 2020
aHUS and kidney transplants is an important research topic for aHUS patients with end stage renal failure. aHUS alliance Global Action has featured several research studies of aHUS transplants, including those by the Zuber Group (Article 330)and Seidlecki Group ( read HERE ). The important outcomes when aHUS is involved are how well the kidney works and how long it will work for.
A recent study released by the Jose Portoles group from Madrid, Spain adds new insights for aHUS patients about the topic.
Its title is “Characteristics, management and outcomes of atypical haemolytic uraemic syndrome in kidney transplant patients: a retrospective national study ” click here for full article.
The study group undertook a retrospective study of kidney transplants , or KTx as the clinicians refer to it , involving aHUS in the years 2013 to 2017. In that time remarkably over 14,000 KTx took place in Spain and there were on average almost 30,000 patients with functioning kidney grafts. Out of those totals only 36 aHUS KTx were found in the national databases.
The group sub-categorised the 36 patients into those whose aHUS was known about before their KTx ,called “recurrent”, and those with a new incidence of aHUS following KTx , called “de novo“. There were 14 recurrent and 22 de novo patients. The de novo group was further subdivided into early onset ( within one month of transplant ) of which there were 16, and late on set ( after one year) of which there were 6 patients.
The patient characteristics, treatments and outcomes of each of those in the three cohorts are detailed in Tables 1 to 3 in the above article.
In the recurrent group, i.e. the 14 patients who had been diagnosed with aHUS before KTx , nine received eculizumab before the transplant. 5 of those patients were considered to be of high risk of relapse ,and 4 were of moderate risk ( see table of risk classifications below). None experienced relapse, including two of the four patients with moderate risk of relapse , who had their ecuizumab treatment withdrawn in the first year after KTx.
Three of the five with did not receive prophylactic eculizumab relapsed with aHUS, at markedly different timelines from transplant i.e. 2 months, 4 years and 10 years. Two of those who relapsed were rescued with eculizumab and recovered. The other one did not ( eculizumab was not available ) and lost the graft. This patient then had two further KTx , one failing and the second with eculizumab worked successfully.
In the second group i.e. 16 patients with early de novo aHUS after a transplant, no kidney grafts were from living donors. 13 of the 16 received plasma exchange (PEX) treatment on onset and four had full and partial kidney recovery from that treatment.
8 of the 9 who did not respond to PEX were rescued with eculizumab. Of them plus the 3 receiving eculizumab without PEX , 8 ended up with complete remission and 2 with partial renal response. All 10 patients had treatment withdrawn on average 21 days after starting. Those with a complete response had received their eculizumab rescue sooner i.e. within 5 days of onset, compared to 22 days for those whose renal response was partial or none.
The striking insight about this group was that their original end stage renal failure was due to other kidney diseases including Glomerulonephritis, Autosomal Polycistic Kidney Disease, Diabetes Mellitus, SLE and Vasculitis. Their de novo “aHUS” was not a primary TMA but a secondary TMA or “Transplant TMA”. After three years of follow up none of these patients had an aHUS recurrence without eculiumab.
In the final group of six de novo patients whose aHUS occurred more than one year after their KTx, genetic tests on 4 of the patients showed that all 4 had low risk genetic predisposition to aHUS, though their cause of kidney failure like the group above had been down to other kidney diseases. Unlike the other de novo group above, triggers other than KTx were found. In this group eculizumab was administered much later than the group above and three patients lost their kidney graft.
This study has been the biggest concerning aHUS and transplant to date and with the longest follow up. It has provided more insights particularly for those other kidney disease patients whose only experience of “aHUS” is immediately following KTx. Theirs is a Transplant TMA encounter rather than aHUS . Their “aHUS” required only short term rescue eculizumab treatment.
This study goes further into determining the risks of aHUS relapse, or put another way the chances of long term remission, for those with KTx. Some may recall the risk matrix that aHUS Global Action has used before.
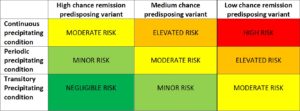
The KTx trigger would fall within the “continuous precipitating condition” but although the Portoles Group would categorise the risks as ” low , moderate to high” from left to right, Global Action describe them as “moderate , elevated and high categories”
But which patients would fall into each category? The risk categorisation used in the study are those with :
HIGH RISK
Previous recurrence
Presence of CFH, C3 or CFB pathogenic variants
CFH-CFHR1 rearrangements
MODERATE RISK
Presence of CFI pathogenic variant
Presence of CFH, C3 , CFB or CFI uncertain significance variant
Homozygosity of CFH-H3 risk polymorphism
Anti-FH autoantibodies
LOW RISK
Isolated MCP pathogenic variant
DGKW pathogenic variant
THBD pathogenic variant
Loss of anti-FH autoantibodies
No genetic findings
Secondary aHUS
More answers are being found to the aHUS Patients Research Agenda question “Is there a significant difference in outcome between having a complement inhibitor before or after a kidney transplant?”
Following this study it is known that:
Transplant can trigger aHUS, but not all Transplant TMAs are aHUS;
When aHUS has been diagnosed prophylactic eculizumab is preferred to prevent recurrence;
When not prophylactic, eculizumab can be effective as a rescue for Transplant TMAs, including aHUS;
aHUS onset triggered by transplant impacts on kidney function and possibly graft longevity
aHUS should be part of any differential diagnosis of any functional impairment following KTz to speed up access to eculizumab if needed
Rescue eculizumab is needed quickly ,5 days or sooner from onset, to get best outcomes
Withdrawal of eculizumab for those with transplants depends on aHUS genetic susceptibility risks, primary kidney disease , extent of ischemic injury to donor kidney, and quality of donor kidney.

