Article No. 303
11 December 2019
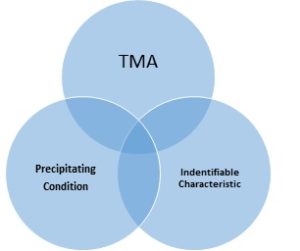
It has taken nearly a century for aHUS nomenclature to reach the level acceptance, application and awareness it has today. But now there are concerns being expressed about its vagueness and its impact on its diagnosis , treatment and prognosis. Instead there is a desire to reclassify all TMAs. So where might existing aHUS patients stand in any such reclassification.
Perhaps a lay view and analysis of the Vienna TMA Group’s TMA categorisation proposal might help with understanding and a definition of what the “new aHUS” community and its patient support groups might embrace.
TMA can be caused by:
1. Anti FH antibodies: Clearly linked to Complement. Some evidence that Complement FH related genetic variants are implicated, but in most cases they are not. So it is primarily an immune disease remedied by reducing the level of these antibodies to a safe level. In the acute phase eculizumab can help. Currently regarded as an aHUS with a reasonable case for it to come under “new aHUS”.
2. MMACHC variant: Mutations in a gene in the liver result in methmaline aciduria and homostystmuria type C , or cblC or more commonly known as Cobalamin Deficiency i.e vitamin B12 deficiency. A relatively common condition which can be acquired in older people but the inherited version is much more likely to show in the very young. It rarely results in a TMA as other symptoms lead to a diagnosis and treatment with supplementary vitamin B12 before it occurs. Two thirds of the few who experience TMA are diagnosed with aHUS and there is a response to eculizumab: but until the vitamin deficiency is resolved, patients may not thrive. Some claim that it is a “pseudo TMA” mimicking TTP or aHUS symptoms. It is primarily a metabolic disease. The case for it to be in “new aHUS” remains open because of the kidney failure.
3. Glomerular: Glomerular Diseases are kidney diseases which damage the Glomerulus in the kidney They include the more common diseases like Diabetes Nephropathy , Systemic Lupus Erythematosus, IgA Nephropathy as well as the rarer forms like MPGN/C3G and Dense Deposit Disease. The extent to which Complement is implicated in each of the them is variable and unclear, though some are more associated with upstream Complement over activity at C3. For there to be a TMA there is some break through beyond C5, needing the use of eculizumab or other Complement inhibitors Not regarded as aHUS at present and little case exists for them to come within “new aHUS” , even with some Complement overlap.
4. Auto immune: There are several common auto immune diseases including Diabetes Type1 Rheumatoid Arthritis where Complement plays a part, but rarely do they trigger TMA. Lupus, anti-phospholipid syndrome and sclerodera are known to be implicated in TMA activity. Those diseases are not regarded as part of current aHUS and there Is little reason for them to be included in the “new aHUS” although in the case of catastrophic APS, Complement Factor H related defects are now thought to be implicated as in anti FH antibody TMA.
5. DGKE variant: Mutations can occur in diacylglycerol kinase ɛ or DGKE. DGKE plays a part in controlling the coagulation system and clotting. When it does not function as it should, a prothrombotic state can follow which can lead to TMA. It is not a part of Complement and not treatable with eculizumab but it has been regarded as an aHUS. Inclusion in “new aHUS” is as open as it is for MMACHC TMA.
6. ADAMTS auto: an acquired antibody version of Thrombotic Thrombocytopenia Purpura or TTP. Something currently that is ruled out as the cause of TMA before aHUS is considered. Not a part of the “new aHUS” but an important partner in the TMA diagnosis journey.
7. Hypertension:Commonly known as Malignant Hypertension, a condition caused by the kidney and which affects the kidney. A kind of renal TMA with hypertension and acute kidney injury present, which has not been generally thought of as aHUS. Treatment with eculizumab can resolve the TMA but not necessarily the hypertension. Recently the role of renin has been identified as having a part in the Complement activation process and the renin inhibitors Askimen at supra dose levels has been used in conjunction with eculizumab to bring about a resolution. As the partial role that renin plays in Complement activation emerges , the stronger the case might become for hypertension TMA to be considered a part of “new aHUS”.
8. ADAMTS Variant: an inherited genetic version of Thrombotic Throbocytopenia Purpura or TTP. Something currently that is ruled out as the cause of TMA before aHUS is considered. Not a part of the “new aHUS” but like ADAMTS auto TMA an important partner in the TMA diagnosis journey
9. Transplant: Transplants create issues for the immune system whether it is a “solid” organ transplant or allogeneic haemopoietic stem cell transplant (HSCT) the latter particularly in an episode of graft versus host disease . Both kinds of transplant can trigger Complement activation and TMA. This is regarded as an acquired TMA, but, as many current aHUS patients have found, there Is still a Complement genetic susceptibility at play too. Particularly when a previous episode of aHUS had unknowingly caused their chronic kidney failure. Donors may be susceptible to “de novo” aHUS if they possess genetic susceptibility. There is strong case for kidney transplant TMA to be embraced by “new aHUS” and powerfully advocated for; but the case for other types of transplant remains open, more needs to be known, particularly about TMA following HSCT.
10. Drug: A number of drugs have a side effect of precipitating TMA. They include immunosuppressants, chemotherapies as well as drugs of abuse or even commonly used quinine. Withdrawing the drug can resolve it but treatment with eculizumab has been found to be effective in some cases if the drug is essential for resolving something more serious. Apart from those in the overlap with a genetic Complement mutation most of the rare instances of drug induced TMA would be outside the scope of “new aHUS”.
11. Complement Variant: The “purest” version of aHUS with a known variant of a Complement component which results in dysregulation of Complement when it is triggered. The mutation can be inherited or new ( but then passed on to the next generation). Treatable with Eculizumab. Those with identified mutations only account for around two thirds of those with a current aHUS diagnosis. The remainder being described as idiopathic. Complement variant TMA will be at the core of “new aHUS”. Already this is also being referred to as Complement mediated TMA in current research publications, and cTMA in shorthand abbreviation.
12. Infection: Infection TMA includes HUS, the typical form, which results from an e.Coli infection. This is more common than aHUS and has been regarded as a different disease, although there is some overlap if a patient is found to have one or more Complement mutations. But there are more infections that can trigger HUS including streptococcal pneumonia, a rare trigger of aHUS and sepsis. HUS by definition excludes aHUS and there is no strong case for it to be included in “new aHUS”. TMAs resulting from other infections might be considered for inclusion, if they are a trigger for Complement variant TMA.
13. Pregnancy: Pregnancy and childbirth are very thrombotic interludes for many reasons. Around 1 in 20,000 pregnancies become problematical because of TMA. The most common causes are pre-eclampsia, eclampsia, HELPP, SLE (Lupus), Antiphospholipid Syndrome , TTP and aHUS. Whilst Complement is being thought a factor in some of the precipitating conditions other than aHUS, research is not definite enough to consider anything other than aHUS pregnancy will come within “new aHUS”. The other precipitating conditions generally have their own patient support network.
14. THBD variant: Thrombomodulin acts with another factor in the control of the coagulation system. Inherited mutations can stop it acting effectively resulting in uncontrolled clotting on the endolethial cells, leading to an uncontrollable Complement activation. Like PLG TMA that follows there is case for THBD to be included in “new aHUS”.
15. Cancer: TMA is not that common in cancer. When it happens it is more often because of chemotherapy drugs and the susceptibility to infections (see those TMAs above ) than the tumours triggering the TMA. Although aHUS Complement variants are rarely found some more common Complement polymorphism have been seen in some cancer/TMA patients. Cancer is very well represented by well-funded patient support networks making very little case for it to come within “new aHUS”.
16. Surgery: Post general surgery (excluding transplants) TMA is a rare occurrence and once identified is quickly treated by Plasma therapy or sometimes eculizumab. Not thought of as aHUS at present but those susceptible due to Complement genetic variants must be a consideration for “new aHUS” , particularly aHUS susceptible living kidney donors in transplant surgery.
17. PLG variant: the PLG gene is responsible for plasminogen to be produced by the liver. Plasminogen is needed for blood clotting. It is part of the coagulation system. Variants in the gene have been found to cause plasminogen deficiency which has been associated with Complement over activation because of its role as a Complement inhibitor. There is currently no treatment available to correct the deficiency. Although a rare contributor to aHUS it could be seen as part of “new aHUS” and more knowledge is needed.
The Vienna TMA Group model has three other TMA categories
a. Plasma Exchange Responsive TMA: A treatment category which is not specific enough for disease classification but may influence first response and post diagnosis protocols.
b. Eculizumab responsive TMA: would also include ravulizumab but like PEX TMA it is not specific enough, although its cost makes it essential that it is not wasted on some TMAs but used when needed for only as long as is needed. Potential application may be more extensive than Alexion’s trials inclusion criteria, and thus, health funding policies permit .Factors influencing TMA remission will become more important. Likely to be embraced by the “new aHUS”
c. Unexplained TMA: Most TMAs have been unexplained at some point. Only TTP preceded the term TMA. They are the “known unknowns” and are yet to be discovered. Take Monoclonal Gammopathy of Unknown Significance, or MGUS, as an example . An inherited benign blood disorder with few noticeable symptoms but sometimes identified in unrelated blood tests when a high level of deformed blood cells or para proteins are spotted. There is usually no need for treatment but, once found, patients are monitored for potential disease development because blood cancers may develop in a few cases. Even rarer, a TMA may happen causing renal damage, sometimes referred to as MGRS , the “unknown” changing to “renal”. It is believed that the paraprotein from MGUS can affect Complement by sticking to CFH and limiting its ability to control complement. A bit like anti factor H antibodies do. Although technically a benign cancer, TMA MGUS would be embraced by the “new aHUS” as a new TMA category
40% of current aHUS patients have no known Complement genetic predisposition but are responsive to complement inhibition treatment. Like MGUS, maybe these unexplained/idiopathic TMA triggers will be explained eventually. Until that time they should remain within the “new aHUS”.
Conditions involving TMA are represented by a range of generic patient advocacy organisations for Kidney Disease, Metabolism Disorders, Thrombosis , Cancer/Leukaemias and Primary Immune Disorders but rarely ,if at all, Complement ( The Russian organisation “Another Life” is the nearest known).
But Complement is implicated in so many diseases not just renal. As well as PNH there are eye disorders like aged macular degeneration, neurological diseases like Alzheimer’s and Parkinson’s, and mental heath disorders like bi-polar and Depression. It all depends which component of Complement is excessive or lacking, defective or hampered.
No umbrella patient support group can be found for TMA.
Some organisations have emerged for more specific conditions like Lupus, Sepsis, Antiphospholipid Syndrome etc. Such organisations tend to focus on the more common forms of the diseases, and as TMA may only impact on a very small cohort in some of these conditions, there may be little attention given to them. Rare disease organisations like those for TTP or aHUS are much more likely to emphasise TMA and treatments like eculizumab/Ravulizumab.
If there is to be a “new aHUS”, Patient organisations should extend their scope to advocate in detail for those conditions out with the “purest” form of aHUS i.e. Complement variant TMA ,or cTMA. From the above analysis the following TMA categories might fall within the scope of “new aHUS”.
| TMA | Included | Abbreviation | ||
| 1. Anti FH anti bodies | Yes | afacTMA | ||
| 2.MMACHC | Probably not | |||
| 3. Glomerular | No | |||
| 4. Auto immune | No | |||
| 5. DGKE | Probably not | |||
| 6. ADAMTS auto | No | |||
| 7 Hypertension | Probably | HcTMA | ||
| 8 ADAMTS variant | No | |||
| 9. Transplant | Yes | TxcTMA | ||
| 10. Drug | Partially | DcTMA | ||
| 11.Complement variant | Yes | cTMA | ||
| 12. Infection | Partially | IcTMA | ||
| 13. Pregnancy | Partially | PcTMA | ||
| 14. THBD variant | Yes | ThcTMA | ||
| 15. Cancer | Probably not | |||
| 16. Surgery | Partial | ScTMA | ||
| 17. PLG variant | Yes | PLGcTMA | ||
| a. Pex responsive | Yes | PexcTMA | ||
| b. Eculizumab responsive | Yes | EcucTMA | ||
| c .Unexplained | Yes | icTMA | ||
| add. MGRS | Yes | MGcTMA |
This is just a lay analysis from an aHUS patient organisation perspective. Others will no doubt see it differently and disagree. Haematologists at the 2019 ASN conference more likely to use TMA preceded by an abbreviation for type of TMA. Losing the “kidney” connection in the name might be a step too far! So how about UcTMA or KcTMA. In the end it will come down to spelling out the definable “identifiable characteristics” of what constitutes “new ahUS”.
There is much more debate and discussion needed before a global consensus is reached. The difficulty will be in the “Ah buts”. When consensus is nearly reached there is always a “Ah but what about…..?”.
It going to be a difficult period for patients, old and new, as a transition takes place. Maybe even causing some confusion, which is a concern when a diagnosis is needed and should an appropriate treatment be delayed. Although it can be argued that there Is currently a lack of clarity and specificity creating barriers to diagnosis.
But change is going to happen, as has been the case in the past. This series of articles has attempted to explain why change might be needed and what it might result in, but it is not definitive. But something will emerge to describe the “new aHUS”at the centre of the diagram below.
Having some early awareness could be of help for whenever it does happen, particularly for practical matters of importance to patients.
Part 2
Part 1
,

