What’s involved in aHUS genetic testing, and are all labs alike? The answer to the first is quite complex, and no – what’s on offer regarding clinical diagnostics, mutation screening, and complement panels vary greatly. The aHUS Alliance Global Action team connects internationally with clinicians and researchers, offering an aHUS network resource for physicians as well as a roster indicating known aHUS/TMA study centers. As a rare form of thrombotic microangiopathy, atypical HUS often found to have a genetic flaw as its root cause.
As part of the University of Iowa system, the team at MORL has partnered with the USA’s aHUS Foundation (formerly the Foundation for Children with Atypical HUS) to host aHUS family conferences for many years. Videos from those meetings have included Dr Carla Nester answering “What is aHUS?” and presenting on the Challenges of aHUS Diagnosis (see also our aHUS Clinical Channel playlists from the 2014 and 2016 family conferences). Dr Richard JH Smith, director of MORL, presented basics of the MORL genetic screening process to families as early as a 2013 aHUS conference. While much more is now known regarding advancements in genetic testing and a better understanding of atypical HUS, what hasn’t changed at MORL is their team’s commitment to excellence and their drive to discover more which will help fill in existing gaps in aHUS knowledge. Dr Smith was kind enough to offer us this comment:
“While we have learned a great deal about aHUS and persons with this disease have witnessed transformative changes in their lives, there remains much to learn. The questions are more sophisticated and subtle, and often very difficult to answer. Scientists at the MORL are dedicated to finding these answers and further improving the lives of persons with aHUS.”
The Molecular Otolaryngology & Renal Research Laboratories (MORL) at the University of Iowa has two lab divisions, the Clinical Diagnostics Division and the Research Division. The MORL Clinical Diagnostics Division is a not-for-profit academic laboratory that focuses on non-syndromic hearing loss as well as complement-mediated renal disease (like cm-aHUS). MORL offers a wide variety of functional tests of complement activity, including measures of complement proteins, the detection of autoantibodies to different proteins (like factor-H autoantibodies), and mutation screening of all genes implicated in the thrombotic microangiopathies (TMAs). Unique to MORL is their commitment to holding weekly multidisciplinary meetings attended by clinical experts, research scientists, bioinformaticians, human geneticists and genetic counselors. This extra level in aHUS genetic screening enables MORL to interpret the results in the context of the provided clinical data and often offer to clinicians, a patient-specific interpretation of the results.
We appreciate the fine work done at MORL in both their Clinical Diagnostics Division and their Research Division. Here’s a selection of articles which focus on aHUS genetics, and which have added to the aHUS knowledge base for academics, researchers and clinicians around the world.
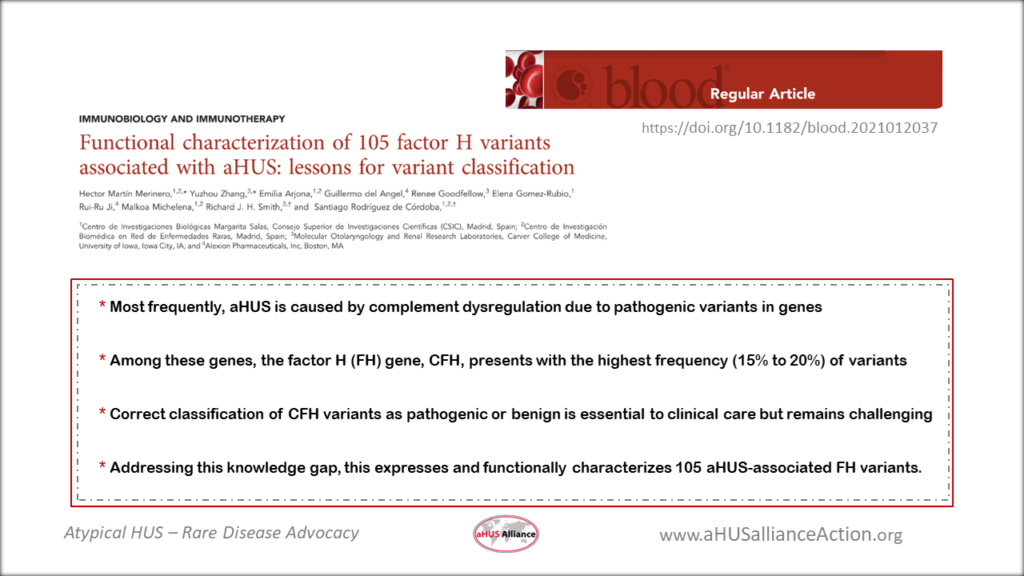
Hector Martín Merinero, Yuzhou Zhang, Emilia Arjona, Guillermo del Angel, Renee Goodfellow, Elena Gomez-Rubio, Rui-Ru Ji, Malkoa Michelena, Richard J. H. Smith, Santiago Rodríguez de Córdoba; Functional characterization of 105 factor H variants associated with aHUS: lessons for variant classification. Blood 2021; 138 (22): 2185–2201. doi: https://doi.org/10.1182/blood.2021012037
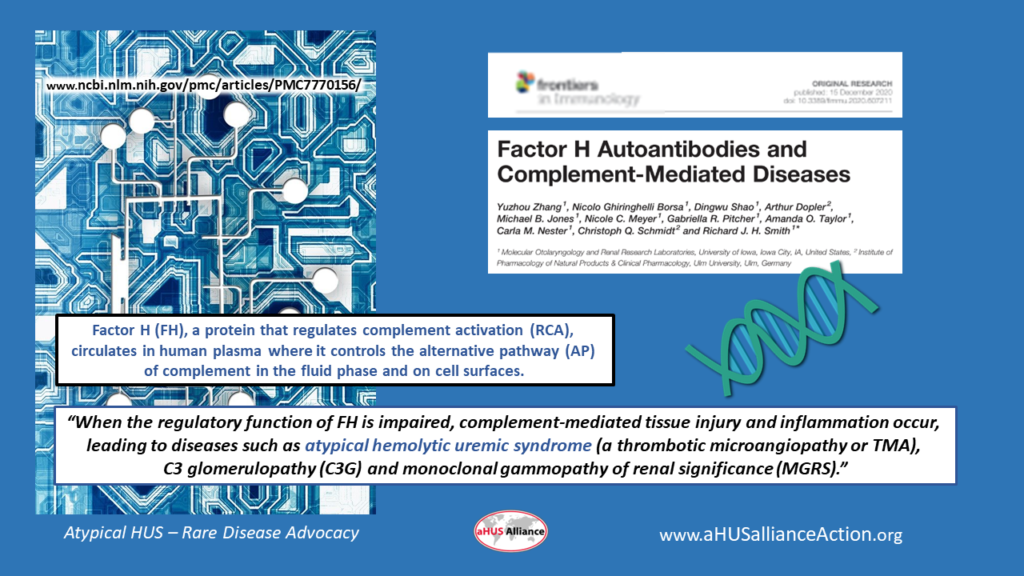
Zhang Y, Ghiringhelli Borsa N, Shao D, Dopler A, Jones MB, Meyer NC, Pitcher GR, Taylor AO, Nester CM, Schmidt CQ, Smith RJH. Factor H Autoantibodies and Complement-Mediated Diseases. Front Immunol. 2020 Dec 15;11:607211. doi: 10.3389/fimmu.2020.607211. PMID: 33384694; PMCID: PMC7770156.
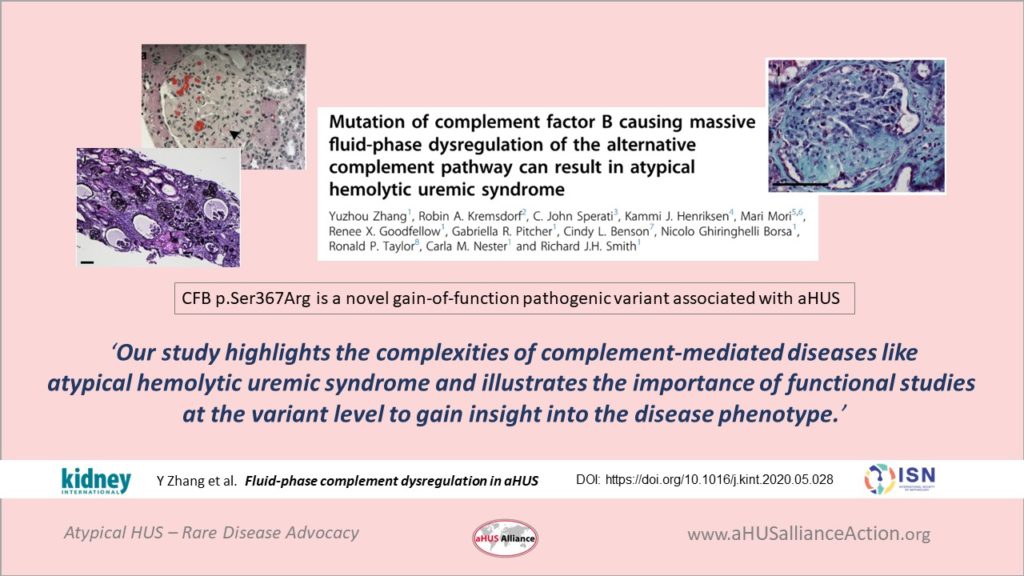
Zhang Y, Kremsdorf RA, Sperati CJ, Henriksen KJ, Mori M, Goodfellow RX, Pitcher GR, Benson CL, Borsa NG, Taylor RP, Nester CM, Smith RJH. Mutation of complement factor B causing massive fluid-phase dysregulation of the alternative complement pathway can result in atypical hemolytic uremic syndrome. Kidney Int. 2020 Nov;98(5):1265-1274. doi: 10.1016/j.kint.2020.05.028. Epub 2020 Jun 12. PMID: 32540405; PMCID: PMC7606633.
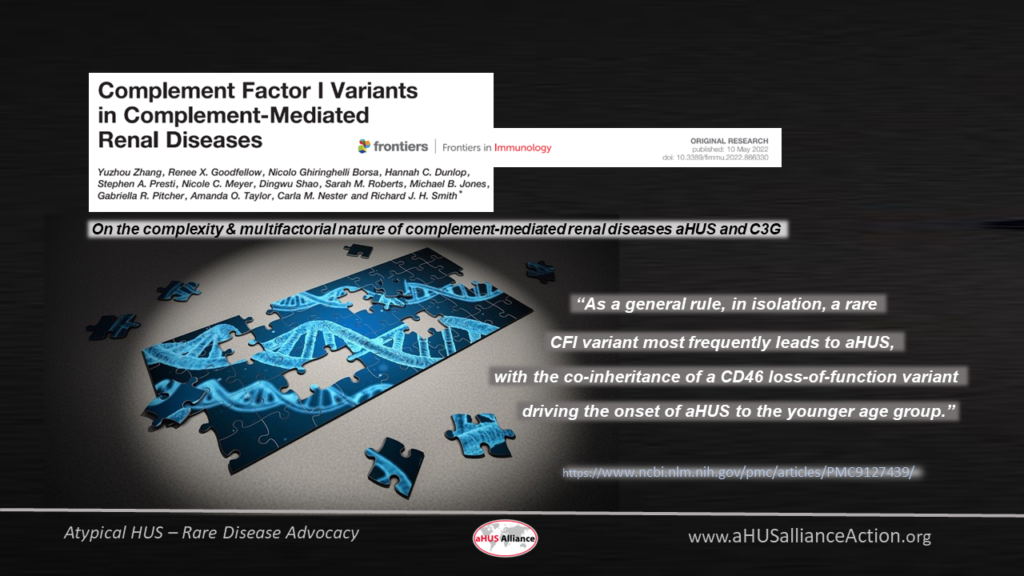
Zhang Y, Goodfellow RX, Ghiringhelli Borsa N, Dunlop HC, Presti SA, Meyer NC, Shao D, Roberts SM, Jones MB, Pitcher GR, Taylor AO, Nester CM, Smith RJH. Complement Factor I Variants in Complement-Mediated Renal Diseases. Front Immunol. 2022 May 10;13:866330. doi: 10.3389/fimmu.2022.866330. PMID: 35619721; PMCID: PMC9127439.

