The topic of ‘changing the name of aHUS’ crops up regularly, so since people keep asking here are details which might help to greater clarity and understanding to this topic.
Question:
Why is there discussion about changing the name of atypical HUS to something else, and how would it really matter?
Short answer: No people or groups are considering ‘changing the disease name’ from aHUS to a single other name.
Answer with a bit more detail: There are however groups of clinician/researchers who note that aHUS is better viewed as a group of conditions, or aHUS as subtypes along a spectrum.
“In Reality” Answer: Researchers have narrowed the knowledge gaps, and some patterns are emerging. It looks like personalized medicine will be the future of aHUS treatment, with certain drugs provided with tailored care plans, will provide better patient outcomes. Expect this to take years to implement.
Let’s walk through a straightforward overview that may help shed light on the needs for, and benefits of, refinements and updates to nomenclature and classification of aHUS (and TMAs).
Updated Classification & Nomenclature
When we talk about classification, we mean how diseases are organized based on shared features. Nomenclature refers to the labels or language we use to describe them.
What we’ve called “atypical HUS” is increasingly understood to be a spectrum of related but different conditions. As new therapies are developed, clearer categories and better terminology will help ensure each patient receives the treatment most likely to work for their specific subtype.
Done with other Medical Conditions: It’s Time for aHUS
Medicine often starts with broad categories, then refines them as knowledge grows.
Other medical fields have already moved toward more precise classification systems, recognizing that better definitions improve treatment decisions. Rare diseases like aHUS sometimes lag behind simply because there are fewer patients to study. Now, growing research and deeper understanding are prompting experts to reconsider whether one broad label can capture the full spectrum of this condition.
Medical knowledge doesn’t stand still — and neither should the language we use to describe disease. Many conditions have been reclassified as science uncovered differences that matter for treatment and outcomes.
When Science Outgrows the Name
If you’re wondering if other medical conditions have reached this same crossroads – yes, and it’s often more visible to the public when new treatments reach the medical marketplace.
Here’s a set of 3 examples where broad terms have been replaced by more precise ones:
Psoriasis – For a long time, “psoriasis” was used as a catch-all label for a family of related but meaningfully different skin conditions. A common and chronic autoimmune condition, it affects millions (about 2-3% of people worldwide). As researchers and clinicians looked more closely, they realized that not everyone with psoriasis had the same disease — the patterns, triggers, and affected populations were distinct enough to deserve their own names. Today, ‘plaque psoriasis’ has well-established biologic therapies, and ‘psoriatic arthritis’ has its own targeted treatment approvals as well. Other subtypes of psoriasis have remained harder to crack, so those remain under study.
Cancer and Genetics– Let’s narrow this very broad field a bit, and use a particular example of how a patient’s genetic makeup might precisely select best treatment options for a specific individual. As breast cancer research has advanced, new drugs now target specific clinical and/or genetic profiles. Certain drugs work best with subtypes of breast cancer. Take this example: identification of breast cancer subtype HR+, HER2- biomarkers allows doctors to take targeted actions with treatments tailored to individual patient needs. That’s now evolved so now the first question for consideration of oncology specialists has evolved into “What type of breast cancer?”.
TTP: Similar characteristics with aHUS – It’s understandable as to why it’s difficult for physicians to distinguish atypical HUS apart from a diagnosis of TTP. Thrombotic Thrombocytopenic Purpura (TTP) and atypical HUS are two rare diseases which look so alike in an urgent care setting that for much of medical history they were treated as variations of the same problem. In a sense, they are — both belong to the TMA family, both turn the body’s clotting system against itself in small vessels throughout the body, and both can quickly become life-threatening.
Put simply, today TTP is divided into two main types based on why the ADAMTS13 enzyme is missing or not working. It is divided into immune TTP (iTTP), caused by antibodies that block ADAMTS13, and congenital TTP (cTTP) caused by genetic mutations present from birth.
This acquired (immune-mediated) form of TTP accounts for the majority of the patient population with inherited cTTP (also known as Upshaw-Schulman Syndrome) representing only about 5% of TTP cases.
There’s another similarity between TTP and aHUS — not every patient responds the same way to the disease’s current treatment guidelines. For patients with cTTP, the current treatment is plasma infusions — effective but not a true fix. For those with iTTP, treatment has improved and utilizes plasma exchange but with steroids, rituximab, and caplacizumab. However there appears to be a problem within treatment of immune TTP (iTTP) — 41–74% of patients relapse; some don’t respond at all (Selvakumar S, Liu A, Chaturvedi S, 2023). With this division into two types of TTP, this work seemingly has just begun as it remains unclear about differences which cause non-responders and relapse risks. More advancements in knowledge must close current gaps.
The evolution from one umbrella term to a more precise, subtype-specific language reflects exactly what good medicine looks like as it matures: the more carefully we look, the better we can treat each person as an individual rather than a category. Where does this leave the topic of atypical HUS nomenclature and classification?
One Name, Many Realities: Why aHUS Needs Clearer Definitions
There seem to be distinct differences within the atypical HUS community regarding patient clinical profiles, patient genetics, and patient responses to treatment. Here are a few instances that suggest different subtypes of aHUS: Some aHUS patients trigger at as very young children, others experience their first onset of disease activity half a century (or later) into their lifespan. Some people experience aHUS as a chronic illness, while other people have aHUS in episodic form with lab values that indicate extended periods of disease dormancy.
Some patients historically labeled as “aHUS” have thrombotic microangiopathy (TMA) where complement activation may be secondary — not the root cause. Treating these patients with a complement blocking drug might not fully control the disease because the underlying trigger is something else (such as an autoimmune disease or pregnancy) . A small subset of aHUS patients have mutations in the DGKE gene and since complement overactivation isn’t the main problem, complement inhibitors often provide limited or inconsistent benefit in these patients.
More data must be collected and much remains to be studied regarding relapse risk for aHUS patients, which includes drug level troughs and complement level monitoring as well.
In a nutshell, we need: A) move away from a ‘one size fits all’ name of aHUS and move toward sort out clearer language which to better aHUS subtypes, B) name these with specific and consistent terminology, C) personalize an optimal therapeutic treatment plan for each, and finally D) tailor ongoing management (and monitoring) according to precisely what works best for an individual’s clinical profile and their aHUS subtype.
Determining the Path Forward: aHUS Controversies
The single term “aHUS” has become outdated because it groups together patients who may have very different underlying causes and treatment needs. More precise grouping and naming will guide more personalized treatments and better outcomes for people across the aHUS spectrum.
Information and resources regarding atypical HUS has been filed under a variety of names and a stockpile of abbreviations. No matter whether the key search terms are ‘complement mediated disease’ or ‘Primary TMA’ or abbreviations which include ‘cmTMA’ or ‘caHUS’ one thing is abundantly clear — there’s little agreement regarding what to call this rare disease.
That’s why the KDIGO Controversies Conference on Complement-Mediated Kidney Diseases: Atypical HUS and C3 Glomerulopathy / Immunoglobulin-Associated MPGN will be convened in Rome in April 2026. You’ll note that the word “Controversies” figures largely in the conference title, and that’s no mistake. Experts in atypical HUS research and clinical care will gather to not only discuss new findings and ‘best practice’ guidelines, but also to argue the finer points of how to update aHUS classification and nomenclature to reflect medical advancements.
We look forward to learning how the controversy unfolds, and encourage people to look deeper with the resources offered below.
Setting the Groundwork: NFK working group,Key Issues & Ideas
Nester CM, Feldman DL, Burwick R, Cataland S, Chaturvedi S, Cook HT, Cuker A, Dixon BP, Fakhouri F, Hingorani SR, Java A, van de Kar NCAJ, Kavanagh D, Leung N, Licht C, Noris M, O’Shaughnessy MM, Parikh SV, Peyandi F, Remuzzi G, Smith RJH, Sperati CJ, Waldman M, Walker P, Vivarelli M. (NKF Working Group) “An expert discussion on the atypical hemolytic uremic syndrome nomenclature — identifying a road map to precision.” Kidney International. 2024 Sep;106(3):383–392. DOI: 10.1016/j.kint.2024.04.016 | PMID: 39089534
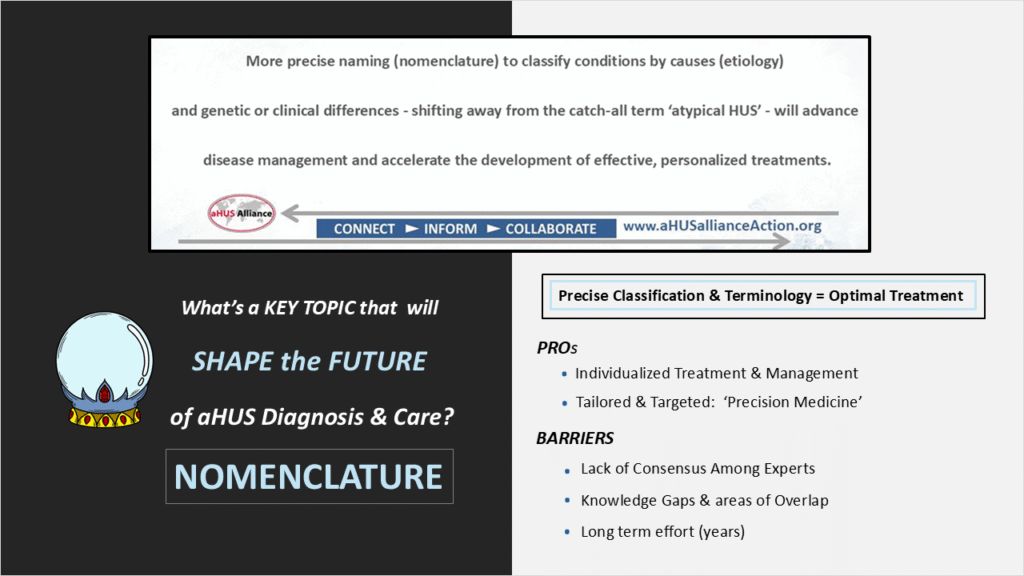
aHUS Alliance Global Action – Revising aHUS Nomenclature
Action Steps: Issues & Problem-Solving
aHUS Nomenclature: Bridges to the Future
Where to Start
Pregnancy Associated TMA: a Start to Nomenclature Revision
What’s in a Name? (articles)
Why the term ‘atypical HUS’ may be ending: aHUS, is its End really Nigh? v3
From our Website Search Bar, keyword ‘Name”: list of 235 articles
USTMA video, Aug 2025: aHUS Advocacy, Patient Groups & Nomenclature (speaker Linda Burke for aHUS Alliance Global Action, ORCID.org #0009-0004-4334-1902)

