Article No. 450
2 August 2021
The more that is known,the more it seems there is to be found out. aHUS research fits into that.
There is aHUS and there is “aHUS”.
When aHUS is mentioned these days there is a need to think “what type of aHUS is being talked about?”
Thrombotic microangiopathy, or TMA , is the common disease mechanism. It is the same for TTP or HUS TMAs too, but it does not mean that those diseases are aHUS.
COVID can trigger an “Infection TMA” , but it does not mean it is HUS or aHUS, unless a genetic mutation in complement is implicated and complement overreacts, then it can be aHUS.
Lupus can trigger a TMA, but it is not aHUS, it is one of the auto immune TMAs. But complement can be a partial cause of the damage to the blood vessel linings, the endothelium. Should Lupus patients become aHUS patients too?
There are coagulation system TMAs where defects in parts of the coagulation system result in unneeded and uncontrolled clotting and damage to blood vessel linings.They are not aHUS. But some coagulation conditions can compromise control of a patient’s complement,which when it is uncontrolled becomes the cause of damage to the endothelial cells, so is it aHUS?
aHUS is synonymous with unregulated complement, but it is defined by complement’s damage to the linings of blood vessels, particularly to the kidney, that triggers the coagulation TMA response . Damage which requires the coagulation system to get involved to protect the blood vessel linings while they repair themselves.
In HUS the damage to blood vessels and intestines is caused by toxins released by the e.coli virus. The damage results in the same coagulation response as aHUS.
Again that response happens with the COVID 19 virus, which directly or indirectly through other immune system responses, inflames and damages blood vessels and the linings of the lungs,
In aHUS it is complement that damages blood vessel linings. Particularly in the kidney. Without kidney involvement it is not aHUS but “aHS”, it is just a complement mediated TMA, with perhaps other organs involved. Should those organs be mentioned?
Complement becomes uncontrolled because of genetic defects in the control parts of complement, which are there to stop any over action and self damage ( it is an irony that “aHUS warriors” fighting aHUS are effectively trying to fight themselves from damaging themselves!).
But perfectly good complement can go out of control because something else in the blood is hampering it working effectively. More and more of these hampering conditions are being identified to explain some of the TMAs created by complement..
Also it is being recognised that, although non complement mediated TMAs are related to specific conditions, complement can be over activated at the same time and be a partial cause of the TMA being triggered. There is a spectrum of TMAs with varying preponderance of complement involvement .
Only Complement Activation >
| <———————————SPECTRUM OF TMAs ——————————> |
< No concurrent Complement Activation
This is is why the clinical community is trying to be more specific in defining each TMA.
The overarching issue for the aHUS patient of course is whether a complement inhibitor like eculizumab can help stop a TMA because of complement playing its part. But what about other disease patients.
Complement inhibition does not work for TTP or HUS TMAs because it is not complement that is causing them.
A new trial announced earlier this year ( more details HERE) will attempt to determine the part, if any, played by complement across the spectrum of TMAs.
Its title is “Diagnostic and Risk Criteria for Complement Defects in Thrombotic Microangiopathy and Amplifying Conditions, Such as Severe Hypertension: The COMPETE Study.”. It is being undertaken by the Maastricht University Medical Centre in The Netherlands who aim to recruit 42 participants.
The outcomes to be measured include firstly – the prevalence of complement-mediated TMA along the spectrum of TMA in the participants over one year.
The trial will also examine the HMEC1 test of TMA activity at the start of the study and after one year.
The ex vivo formation of C5b9 (membrane attack complex which damages the endothelium ) will be examined for changes each month during a year of monitoring each TMA.
The C5b9 formation will be compared with other routine complement measures at the same time.
What happens to the kidney will also be measured , eGFR and whether end stage failure is reached, for the diagnostic and prognostic value of blood measures and kidney biopsy.
Finally the TMA end point and prognostic value of genetic testing will be assessed.
It will be two or three years before the results of this study are known.
Participating patients in those TMAs
-without any complement involvement, they will not have aHUS and their current disease name retained, with maybe a renamed sub cohort which suffer TMAs
-with only complement involvement, they will have what is now known as aHUS, if there is renal damage.
– with only complement involvement but no renal damage, they will need a new name,
– with partial complement involvement , from dominant to minimal levels, will need to be carefully named.
The latter will need careful renaming because complement , although not completely involved, may be down to genetic defects, or if not, something is hampering the control it usually has.
This category of patients may need their complement to be inhibited or modulated to stop the membrane attack complex causing endothelial damage. They will also need treatment for what is causing the hampering of complement control.
When drugs are trialed and approved, it is for a specific health condition. The approval decision for eculizumab to be used for PNH did not mean that it was approved for aHUS. That was done separately but only for a specific TMA- aHUS. Not HUS, nor Lupus TMA, nor Bone Marrow Transplant TMA and others , as such patients were excluded from the trial. But those patients might have benefitted. So in the future proper definitions may help more access to drugs , more demand should impact on price.
Things have become more complicated with time but the key purpose of aHUS advocacy is to see all patients treated with complement inhibitors like eculizumab , ravulizumab and crovalimab when needed for as long as is needed.
Another is to raise awareness of aHUS, as awareness is important to diagnosis.
If our disease is to be reclassified and renamed with new abbreviations, there will still be a need for a link from the old to the new to avoid confusion. However this will present an opportunity to address the “HUS” usage. Conrad von Gasser never intended that HUS should only refer to those TMAs brought on by e.coli , others have done that.
The HUS patient community regards e.coli as its enemy, and may well welcome their life threatening condition featuring the cause of it in its name at last, e.coli to become E.coli HUS or e.cHUS, with maybe the S being replaced by D for disease now that the cause is known. E.coli HUD might mean more to the general public, who need to know about the consequences of poor hygiene if e.coli is to be less of a problem to society.
This permits the “new” aHUS to drop the atypical ( it has been too loosely used rather than was the original intention just to convey that it was not the “typical” e.coli version) and it could become something like Complement mediated HUS, cmHUS? , the one in which :
– complement causes endothelium damage ,wholly or predominantly;
– complement causes damage because of genetic defects in complement , or an external hampering of its control;
– renal injury is evident;
– and a suitable complement inhibitor works effectively?
A name which specifically describes “cause” and “effect”
There is no doubt that today a “ new iconography” is needed much as was the case in the HUS and TTP classification debate in the late 1980s/ early 1990s, because of an emerging “babble of names”.
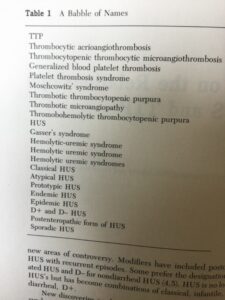
Extract from Chapter 3 of the book “HUS and TTP” edited by Kaplan, Trompeter and Moake published in 1992.
Today’s “babble of names” goes way beyond those for HUS and TTP because of genetic research since. ADAMTS 13 in the case of TTP and the discoveries around the impact of complement in HUS. Those causes and mechanisms might have been suspected but were not known 30 or more years ago.
Even so, back then, HUS and TTP were seen as part of the “TMA family” much as “lions and tigers are recognisable as different animals”, but are a part of the “ cat family”. At that time HUS/ TTP classification was an attempt at an atypical classification . aHUS was, and remains, much more than a “liger”.
The Maastricht University study will contribute to, and help, the new iconography debate. This debate must not be a matter of semantics for its own sake but one of practicality, done to give clarity, consistency and timeliness to the diagnosis process. It must also result in specific disease or syndrome identification for better targeted treatment all round. Quicker and more accurate identification of the manifestations of the diseases.
When this blog was nearing its final draft aHUS alliance Global Action learned from social media that the National Kidney Foundation in the USA has decided that is going to rename our global disease and has set up working parties of clinicians to do so.
The debate appears to exclude the aHUS patient community, within, and outside of, the USA.
As always Global Action welcomes thoughts and comments about changing the name of our disease, including its necessity or any concerns about what such changes might bring.
aHUS alliance Global Action has featured articles about aHUS nomenclature for several years. See a selection of published articles on the topic
TMA-SEMANTICS ARE IMPORTANT
AHUS IS ITS END REALLY NIGH? (PART 1)
…implications are for patients and patient organisations ,if or when aHUS is replaced, will be addressed in part 2 and 3 of “aHUS is its end really nigh”. …
AHUS IS ITS END REALLY NIGH? (2)
Article No 300 4 December 2019 In Part 1 the 95 year journey for aHUS to become in common use to describe our disease was sketched. The name has…

