It’s a casual question people ask all the time, “How’s it going?” and the usual response is “Fine”. Even when that’s not true. Challenges continually appear in life, and it’s stressful to find your way around obstacles. While everyday life includes some degree of stress, and perhaps scattered episodes of anxiety or depression, if those emotions are intense or linger it’s vital to seek professional help. Often it’s more of a cumulative effect, with lots of little issues that can build to make people feel anxious or depressed. When reality dawns and you’re faced with matters you can’t control, what’s your fallback? How do you cope? What’s available to you for support, whether it’s from friends and family, faith groups and service clubs, or counseling? Do you feel you’ve developed a strong personal ‘toolkit’ of ideas, techniques, and options that can help you ‘bounce back’ in tough times? We’ll admit to being among the many who could use a little help at times, in a few areas.
Since the journey and pathways in our lives can’t always be sunny and smooth traveling, it’s more a matter of knowing what you personally can do and what ‘works’ for you as you navigate life. It’s different for everyone. Many people feel that a continual roller-coaster of emotional highs and lows is exhausting, so their discovery of finding more balance is a relief. Others acknowledge when things are beyond their control, and work to move past their feeling of helplessness through building skills and coping techniques. Swirling thoughts and the general unease of anxiety can be a fear that mounts to become a crippling force for some, and getting stuck in that whirlpool can makes breaking free difficult. Others experience layers of difficulty that build up from matters big and small, until the weighty blanket of depression dampens enjoyment and deadens productivity of goals or numbs their daily life. At such points, recognizing signs of distress is an important first step to begin seeking more positive pathways – but how?
Multiple components unite to create a sense of well-being, which usually is considered to be a blend of physical health with emotional, social, and psychological wellness. Having strength and resilience are attributes which cut across all these areas, so this article touches upon each to provide insights to consider and resources to delve deeper. Many people already utilize, or at least have some degree of knowledge about, various building blocks that can help create a strong personal foundation. As children we were guided by parents and teachers to take care of ourselves with proper nutrition, enough sleep, and the importance of ‘Golden Rule’ aspects which were simply worded but proactively thoughtful and related to having goals and being kind. In today’s world, the term ‘self-care’ in its purest form means exactly that – keeping an awareness of how you feel, think and act and noting what negative factors impact your mental wellness. ‘Self-care’ isn’t an indulgence, nor the promotions seen during television commercials or magazine ads, it’s taking stock of all aspects of you as an individual and learning what personally is needed for support and enrichment in your daily life. Stress impacts you physically, so we’ve included potential aspects to consider in that regard as well.
Mental wellness is an ambitious topic, but one worth tackling. Here’s an overview to start your journey of self-discovery, and we encourage you to explore more through reading and through speaking with professionals in fields such as counseling, therapy, cognition specialists, mindfulness/spiritual practitioners, behaviorists, or nutritionists.
(Disclaimer: Material referenced in this article is neither endorsed nor recommended. As an overview, it does not provide complete information nor professional and verified content. Contact your medical or mental health team for specialized and accurate information specific to your situation.)
Mental Wellness: Why this topic Now?
Wondering why a rare disease community would tackle the subject of Mental Wellness? And why now, regarding the timing of this topic?
A rare disease diagnosis affects not just the patient and all areas of their life, but impacts their family as well. Stress can build up from multiple areas of life: economic burdens, lost time at work or school, changes in lifestyle, shifts in relationships, a sense of isolation or lack of understanding from others, circumstances which lay siege to your usual ‘sense of self’, and myriad more aspects. Atypical HUS advocacy has often addressed components of mental wellness over the years, to include a 2014 video created and produced by an aHUS family caregiver, in association with clinical psychologist Dr Jody L Jones and titled Rare Disease Challenges: Support for Patients & Families. Some of our articles have been topical, such as our feature on COVID and Mental Health. Most have more broadly addressed general mental wellness, such as articles on the Zen of living with a rare disease, the many aspects that impact our sense of well-being, or being a family caregiver. Over the years* we’ve woven Mental Wellness threads into our aHUS advocate efforts as part of our ongoing design to provide insights, support, and informational resources. (*see a small selection of these within ‘Resources & Assets’)
Often people can feel overwhelmed by the pressure of rare disease challenges, which can seem to come from multiple directions at once, and where no one seems to understand your experiences. It’s even more difficult when you feel like no one is listening, or that others skim over your words with platitudes or advice. Here’s light-hearted look at that type of communication flow.
Video by Jason Headley (1:41 minutes)

Click Title to Watch (or Click HERE)
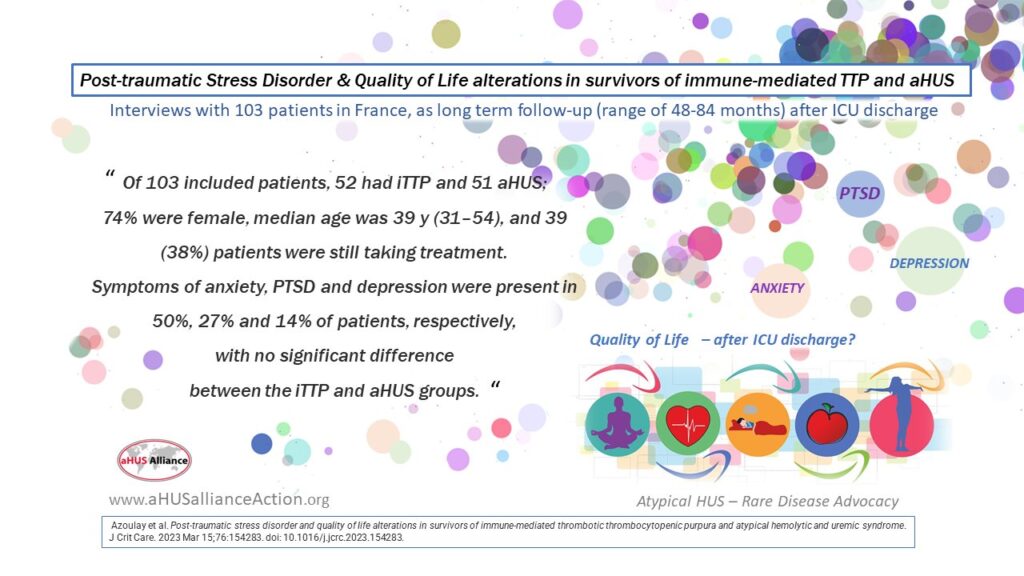
Why in particular are we featuring an article on Mental Wellness now? Although it will be featured in the upcoming August 2023 vol 76 Journal of Critical Care, we noticed a new publication going to print, and highlighted this research about post-traumatic stress disorder (PTSD) and aHUS/TTP patients on our 10 April @aHUSallianceAct Twitter feed. Since one of the key goals for our aHUS Alliance Global Action team is to share information across social media platforms, and this wasn’t published with Open Access to content, we designed an image we felt would convey the importance of this research to aHUS families (our apologies to the publication’s authors)
Azoulay et al. Post-traumatic stress disorder and quality of life alterations in survivors of immune-mediated thrombotic thrombocytopenic purpura and atypical hemolytic and uremic syndrome J Crit Care Vol 76 2023, 154283 https://doi.org/10.1016/j.jcrc.2023.154283.
This publication was based on a French study of 103 patients, 51 with aHUS, and focussed on ‘quality of life alterations’ in survivors of immune-mediated TTP and atypical HUS. Both iTTP and aHUS patient groups experienced symptoms of anxiety, PTSD, and depression with no significant differences between the patient groups. Data was gathered from patients who were interviewed following a lengthy period after they had been discharged from an intensive care unit (followed up between 48-84 months after ICU) and asked questions about their Quality of Life. As aHUS can a life-threatening condition that may occur without warning and be serious enough to indicate a stay in an intensive care unit, it’s not surprising that aHUS families would have a keen interest in dealing with aHUS in the long term or that patient comments about anxiety and depression would occur efforts such as our 2022 Rare Disease Day project.
While people experiencing traumatic events in their life does not necessarily equate to a diagnosis of post-traumatic stress disorder, it is beneficial for them to know about PTSD and to learn more about its signs and symptoms and ways to treat it. Some weeks after sharing the Azouley et al image on our social media, an aHUS Families Conference in Baltimore listened to therapist Stephanie Huhn (MA, LLP) address issues of anxiety, depression and trauma. Knowing how to seek help, as well as being mindful of your emotions is key, as is giving attention and balance across all areas of personal health: physical, emotional, social,spiritual, and intellectual. Mental wellness is an issue that cuts across geographic borders and has long been identified by aHUS advocates,indeed featured as one of 15 points in our global aHUS Patients’ Research agenda. “Does the anxiety and self-esteem of aHUS patients vary significantly between treatment types and what can be done to reduce and boost them respectively?”
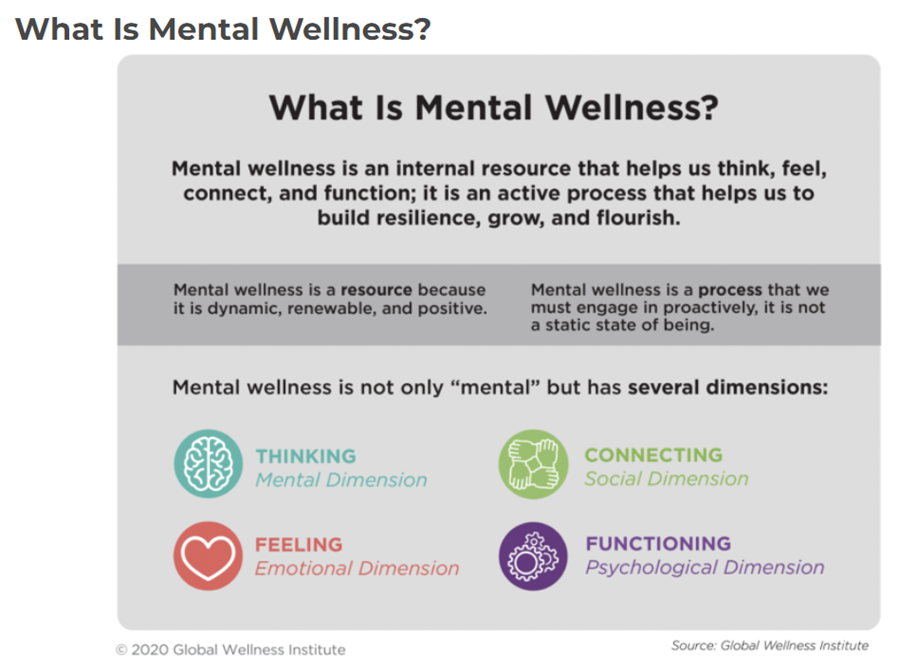
Components of Mental Wellness: Thinking, Connecting, Feeling and Functioning
If you search online to better understand the term ‘Mental Wellness’ you’ll find a wide variety of definitions. The team at non-profit Global Wellness Institute describes it as, “Mental wellness is an internal resource that helps us think, feel, connect, and function; it is an active process that helps us build resilience, grow, and flourish”. As something that people strive to reach and accomplish, and rather than a one-and-done goal, mental wellness is more of a process that is mindful and ever evolving. In the Global Wellness Institute’s image below, the term ‘mental wellness’ encompasses several dimensions: Thinking (mental dimension), Connecting (social dimension), Feeling (emotional dimension) and Functioning (psychological dimension).
People with atypical hemolytic uremic syndrome almost always experience some degree of damage to their kidneys, which explains why ‘uremic’ is part of the condition’s name. There is a relationship between issues with cognition and poor kidney function, which can create a sort of ‘brain fog’. As we’ve written prior, “Just as with the general public, patients with kidney disease or chronic illness can experience trouble concentrating or may have episodes of forgetfulness. Difficulty with gathering and processing information (among other cognitive functions) can impact students at school or may challenge employees in the workplace. For patients with kidney disease, confusion or memory issues regarding appointments or medication routines may interfere with patient compliance related to medical care. It’s vitally important to note that at times all people can experience degrees of forgetfulness or have periods in which lack of concentration or attention might cause personal, work, or health issues – or vice versa. Stress, diet, lack of sleep, certain medications, and various medical conditions may all affect mental clarity or how individuals take in and process information about the world around them.”
Imagine patients with impaired kidney function realizing that ‘brain fog’ has required changes to their daily functioning or impacted their quality of life – wouldn’t one expect that this would cause stress, with some degree of depression or anxiety? Episodes of aHUS may be few and fleeting, or it may be experienced as a chronic illness. It’s reasonable to expect that the unpredictability of episodic aHUS may cause anxiety while coping with daily life to accommodate chronic illness may not just be challenging but cross over into depression. Patients are people, and just like no case of aHUS is quite like any other, there’s no set course and no one ‘right’ way to strengthen your resilience and expand ways you can cope – and perhaps even thrive.
It’s quite telling that global aHUS community members participating in the 8th annual aHUS Awareness Day project in 2022 (80 patients in15 nations) independently mentioned the word ‘resilience’ as the most commonly held attribute when describing their journey toward this rare disease diagnosis. On an intuitive level, and to a certain degree, we know that’s what it takes to live our best lives despite the uncertainty of living with a diagnosis of atypical HUS. It’s much more challenging, yet of vital importance, to look holistically at the many factors which affect the ways we look at the world and how we live our lives.
Behind its Effect on your Body: the Physiological Response
During stressful times it’s not uncommon to experience bodily reactions such as an elevated heart rate or tense muscles,so let’s look at a few basics regarding these mind-body connections. There’s an undeniable link between living through difficult situations and your body’s physical reaction to challenging events. According to Dr Jill Goldstein, a professor of psychiatry and medicine at Harvard Medical School, stress affects memory as well as other brain functions, to include mood and anxiety, but also promotes inflammatory processes in the body. As noted in that 2021 article published by a division of Harvard Medical School, “Researchers believe that when one part of your brain is engaged, the other parts of your brain may not have as much energy to handle their own vital tasks” and goes on to note “if you are in a dangerous or emotionally taxing situation, the amygdala (the part of your brain that governs your survival instincts) may take over, leaving the parts of your brain that help to store memories and perform higher-order tasks with less energy and ability to get their own jobs done. ‘The basic idea is that the brain is shunting its resources because it’s in survival mode, not memory mode,” says Dr. Ressler. This is why you might be more forgetful when you are under stress or may even experience memory lapses during traumatic events’.” Common physical manifestations of stress may include headaches, insomnia, back pain, high blood pressure, and weakening of the immune system.
Here’s a brief ‘video snapshot’ from a TEDed lesson, from a longer video on biologic responses on How Chronic Stress Affects your Brain – by Madhumita Murgia
Mental Wellness includes awareness to address emotional and social aspects, but also being mindful of self-care for physical aspects through techniques such as doing a ‘body scan’. Tension headaches, body aches, and upset stomachs can be outward signs of stress impacting your physical health. This can be true across the distress duration spectrum, from temporary stress that’s fleeting, chronic stress that’s ongoing over long periods of time, or for stress ‘triggers’ that link our current world to past discomfort or emotional trauma. Post-traumatic stress disorder (PTSD) is a serious mental health condition in people who have experienced or witnessed a very traumatic experience or set of circumstances, and PTSD is diagnosed by medical professionals after in-depth assessment. The American Psychological Association classifies diagnosis of PTSD as a psychiatric disorder noting, “An individual may experience this as emotionally or physically harmful or life-threatening and may affect mental, physical, social, and/or spiritual well-being.” If daily life seems to provide insurmountable or intense challenges that prevent you from functioning well, or you have disturbing thoughts and feelings, seek immediate professional help.
Anxiety can create a ‘Fight or Flight’ set of automatic physiological responses. While stress is based on response to events or situations that are unpleasant, anxiety is more internal and generally involves your own thoughts reacting to that stress. Scientists have long studied the effect of real or perceived danger in animals of all types, to include how it impacts the human body. A 2019 article explored skeletal hormone involvement as well, in addition to these more commonly expressed concepts “As part of the response, the adrenal glands release hormones including adrenaline, norepinephrine, and cortisol, which triggers the cascade of physiological responses, including an increase in temperature, heart rate, respiration rate, blood pressure, and energy expenditure.” According to the Mayo Clinic, cortisol is the primary stress hormone while adrenaline also has its role in ‘fight or flight’ responses but warns “The long-term activation of the stress response system and the overexposure to cortisol and other stress hormones that follows can disrupt almost all your body’s processes.” That’s a sobering concept indeed.
Others may find that stressful events lead to depression. The Cleveland Clinic describes it this way, “Depression is a mood disorder that causes a persistent feeling of sadness and loss of interest in things and activities you once enjoyed. It can also cause difficulty with thinking, memory, eating and sleeping.” In an aptly titled article, “Anxiety and Depression Have Their Ups and Downs” (Thrive Counseling) depression is described as feeling immobilized or numb, with the tagline ‘freeze and collapse’ response. Whether it’s feeling helpless or detached, or wishing away days or circumstances, depression can leave people feeling stuck while anxiety may be experienced as feeling on ‘high alert’ or by overthinking events or concerns. Learning how to cope: that’s easy to advise – yet it’s more a matter of finding what works for each individual and that involves both introspection and personal growth. It’s important to discover techniques that help you to ‘even out’ or de-escalate emotions into more moderate ups and downs that help you feel more comfortable with your life, and with yourself.
Types of Therapy – Not just a Verbal ‘unburdening’
Taking notice of how you’re feeling can help you understand what triggers stress or anxiety can help you understand what’s needed to establish or regain a sense of well being. For some, circumstances related to life situations such as illness may be beyond their control and cause feelings of helplessness, worry, or frustration. Other people find mixed reactions in social situations or at the workplace, or with certain things causing an increase in stress or emotional upheaval, yet some find community and understanding there to be a centering force. As there’s no single template of ‘what works’, it’s important to look and consider a wide array of assistance and support.
If your first thought of therapy involves a mental picture of sitting down to ‘talk it over’, you’re not alone. Let’s blame that idea of helpful deep conversations on popular culture and go beyond to look at what else is available. While this type of verbal unburdening works quite well for some people, know that there are many different types of therapy to explore and find what works for you.
There are many types of “talking therapy”(NHS) to include: Cognitive Behavioral Therapy (CBT), Counseling, Interpersonal Therapy (IPT), Eye movement Desensitization and Reprocessing (EMDR), and Mindfulness-based Cognitive Therapy (MBCT). Cognitive behavioral therapists work with people in the context of their current situation, concentrating on their life views and beliefs as they explore how to improve their life through changed behaviors. Traditional Counseling is most often what comes to mind when the topic of therapy arises, where people speak confidentially (in private or within a group) to a therapist who helps them find pathways to work out their problems. Interpersonal Therapy is a talking therapy that focuses on working through relationships with family, friends, and others in your life. Some therapies involve lesser amounts of talking, and focus more on non-verbal cues. EMDR is a therapy type often used for those diagnosed with PTSD, and with mostly non-verbal assists it helps the brain ‘retrain’ to reprocess memories of trauma experiences and reduce their impact. Formed as an offshoot of cognitive therapy to address depression, MBCT incorporates mindfulness practices such as meditation and breathing exercises which help people focus on their thoughts and feelings as they happen. Different talking therapies may be more helpful for some problems and conditions,, just as certain types might suit an individual’s style more than others.
Some individuals may find non-verbal therapies more their style, and there are many to choose among. The variety is wide, among them: art therapy, biofeedback, music therapy, creative writing or personal journaling, massage, acupuncture, dance or movement therapy, and play therapy. In some cases, people may find non-verbal mental wellness options will not include much therapeutic terminology, such as with sports or with meditation practices. Options can be explored in the field of complementary medicine, where traditional medical care is supplemented by other therapeutic options such as acupuncture or neurofeedback therapy. Some healthcare practices offer integrative medicine where their providers offer both traditional and complementary treatments, although not all treatment options may be covered by insurance coverage.
Art and other types of creative therapy can assist people by encouraging non-verbal methods to express thoughts and feelings, sometimes ones that are deeper than the conscious levels that talking therapy can access. According to the Cleveland Clinic, music therapy such as listening, composing, or just playing music, can help people cope and reduce stress through self-expression but music therapy also yields physical benefits such as improved memor and lower blood pressure. In frequently cited research by Field et al, massage therapy reduced levels of the stress hormone cortisol by 31% with an increase in certain neurotransmitters associated with feelings of well-being (28% for serotonin and 31% for dopamine). Other publications also suggest that massage therapy by a licensed practitioner helps both your body and mind relax by production of endorphins, serotonin, and dopamine which reduce stress via this mind-body connection.
Children in hospital settings often have access to specialized ‘Child Life’ therapists, whose profession addresses the concepts that: “Infants, children and youth confront a wide variety of stressful and potentially traumatic events that can impact their ability to cope. These experiences related to healthcare can lead to feelings of fear, confusion, loss of control and isolation that can inhibit their development and have negative effects on their physical and emotional health and well-being.” We’d argue that people of all ages could benefit from these tenets of Child Life professionals.
Individuals are Different – a Personalized Approach to Mental Wellness
Health and wellness are two words often linked together, and for good reason. Proper nutrition, sleep, exercise and hydration are often mentioned as physical aspects but which are sometimes overlooked in our busy lives. But there is more to consider, and those concepts are less easy to quantify. Caring for yourself includes other attributes that are sometimes given only passing notice but still are key to mental wellness such as: setting goals, staying connected, keeping positive, and living with an ‘attitude of gratitude’. For some people, mental wellness may include being part of a faith community and considering a ‘meaning-filled life’ either through individual spiritual practices, attending services, or going on a retreat. Time and again we see the rather vague phrase ‘work-life balance’. Yet wellness means not only taking care of the physical body but active inclusion of social-emotional aspects. Have goals or a purpose in life. Help others. Help yourself, and be connected to something bigger than yourself. You’ve heard all of this since you were a young child, but how often have you considered these in your daily activities as an adult? (eg M Pogosyan article, Psychology Today)
Everyone is different, so people need to find what works for them. Those approaches to mental wellness will vary not only with individuals, but with changes over time and within current circumstances. Support your body with proper rest and diet, which includes being mindful and having a ready toolkit to call upon. Incorporate healthy foods during your meals, especially if you’ve been feeling a bit rundown, and are aware you haven’t been eating well. Take a deep breath, and be aware of how it feels to release it very slowly through your mouth. Most will experience a sense of muscle relaxation in the chest and neck areas, releasing tension which may not even have been noticed. Stress and anxiety can be pronounced in university students at exam time, so it’s not surprising that colleges often offer online mental wellness resources that include grounding and breathing exercises to calm the nervous system. Breathing exercises and forms of meditation are practices that people can incorporate into daily life, as a personalized aspect of self care. Meditation has been practiced over many centuries for spiritual reasons, but increasingly people are turning to meditation for its physical and mental health benefits. Meditation helps to reduce stress, improve sleep, and decrease blood pressure. Find what works best for you, whether it’s more spiritual in focus or an aspect which also includes components of physical practice, such as the breathing and mindfulness through tai chi or yoga techniques.
Getting outside and enjoying natural surroundings is a pleasant experience, but nature’s benefits go far beyond that. Regarding the term ‘Nature-Deficit Disorder’ used in Richard Louv’s 2015 book ‘Last Child In The Woods’, M.R. Choudhury wrote in a 2019 Psychology Today article “According to Louv, nature-deficit disorder is not the presence of an anomaly in the brain; it is the loss of connection of humans to their natural environment. Staying close to nature improves physical, mental, and spiritual wellbeing. It makes us feel alive from the inside, and we should not compromise it for recent developments like urbanization, technology, or social media”.
Those with a rare kidney disease like atypical HUS need to be particularly aware of the holistic nature of health in general. Taking dietary supplements you’ve seen on social media or read about online should be discussed with your care team, since overloading the body’s balance or interfering with prescribed medicine can lead to negative health impact. We’ve posted articles with overviews of scientific studies regarding relationships such as sleep disturbances and kidney disease, as well as the connection between kidney and heart health (cardiorenal syndrome). For those living with a rare disease or chronic illness, there are additional layers of concerns which make mental wellness more challenging and some may argue more important to address.
Eating healthfully is something we all aspire to do each day, and ‘fueling’ the body with good nutrition components is a key factor in every aspect of wellness. High amounts of sugar and fat aren’t good nutritional pillars for anyone, and high levels of salt are especially problematic for patients with high blood pressure or kidney disease. ‘Emotional eating’ during times of high stress isn’t uncommon. Dietician Katie McCallum noted the importance of targeting underlying issues or emotions and addressing them instead of using food as a coping mechanism. Studies have shown a link between eating highly processed foods and higher levels of depression and anxiety symptoms. Diets that include anti-inflammatory foods such as vegetables, fruits and whole grains have been studied and initial findings indicate that such a diet may reduce the risk for depression (Belliveau et al, 2022), so be mindful to incorporate healthy foods into each meal and as snacks. Probiotics may improve ‘gut health’ and could help boost mood and cognitive function, although more study is needed. Across 17 studies with over 150 thousand total participants, there seemed a strong link regarding dietary nutrition, foods linked with inflammation, and mental health in a meta-analysis by Li et al (2022) noting “that individuals on pro-inflammatory diets were 45% more likely to suffer from depression and 66% more likely to suffer from anxiety disorders than those on anti-inflammatory diets.” It’s important that your physician is consulted with regard to consideration of any dietary supplements. Seek out a nutritionist or dietician, and speak with your medical team, to create an individualized dietary plan right for you.
Mental wellness is a broad topic with many topics which span physical, social, and emotional components. We’ve offered only an overview here of aspects which we hope provide basic information and general resources. Many of the resources below have additional links and suggested readings, presented to assist your personal journey of positive growth and life balance.
Dig Deeper: Assets & Resources
Wellness articles that are aHUS-Related, from our website
Attaining aHUS wellness and well being (Sept 2020)
Wellness & Well-being: Project for aHUS Awareness Day 2020
The role of Positive Health in the Dutch approach to aHUS (July 2019)
aHUS and the Teen Years (April 2021)
How Do You Define Wellness if You’re Living with a Rare Disease or Chronic Illness? (July 2017)
General Information
Caring for Your Mental Health (NIH: USA National Institute of Mental Health) El cuidado de su salud mental
Mental Health: Feelings & Symptoms (National Health Service NHS, UK)
Chronic stress puts your health at risk (Mayo Clinic)
Your Healthiest Self: Emotional Wellness Toolkit (National Institute of Health)
How to Improve Mental Health (National Library of Medicine, MedlinePlus.org)
Books: Topics in Mental Wellness & Self Care (Reading Well.org, UK)
Mental Wellness & your Physical Body
Getting to Know Your Brain: Dealing with Stress (video, NIMH)
Understanding Depression and Anxiety as a Fight-Flight-Freeze Response (MindFaculty.com)
Good nutrition: an important Stress Management Tool (Univ. Of North Carolina At Chapel Hill)
10 diet and lifestyle tips to help Manage Stress (article by Jo Lewin, Registered Nutritionist)
Eat These Foods to Reduce Stress and Anxiety (Cleveland Clinic)
Hydration and Mental Health: How Are They Related? (Nutrition News: Abbot)
How Yoga helps your Mental Health (Resources to Recover.org)
Don’t be Alarmed, but Your Kidney has a Clock (RenalFellow.org)
How does sleep relate to mental health? (Mind.org UK)
Children & Teens
Stressed out kids? Signs and strategies (Mayo Clinic)
Childhood Stress: How Parents Can Help (Kids Health.org) Estrés infantil: Cómo pueden ayudar los padres
Depression in children and young people (National Health Service NHS, UK)
Mental Health Minute: Stress and Anxiety in Adolescents (video, NIMH)Mental Health in Kids With Chronic Illness (Child Mind.org)
Family & Caregiver Stress
Caregiver stress: Tips for taking care of yourself (Mayo Clinic)
Caregiver Stress & Burnout (Help.Org)
Coping with the Chronic Illness of a Spouse (Brigham Young University)
How to Cope When Your Partner Has a Chronic Health Issue (Very Well Mind.com)
The Other Sibling: A Systematic Review of the Mental Health Effects on a Healthy Sibling of a Child With a Chronic Disease (Mariñez et al, 2022)
The impact of Rare Diseases on Sibling experience (Rare Revolution)
When a Sibling Is Chronically Ill: How it affects his or her siblings (K Virant, Psychology Today)
Talking to Young Children About a Loved One’s Serious Illness (Cleveland Clinic)Talking to your Children about your Condition (National Health Service, UK: Inform)
Rare Disease – Hospitalizations – Kidney Disease: Topics in Mental Health
Rare Disease Patients Are At Risk of Depression and Anxiety (A. Funk 2021 for CLS.com)
Mental Health in Rare Disease: Taking Care of Your Mind & Body (May 2023, Global Genes)
Depression & anxiety in patients with rare chronic diseases Uhlenbusch N et al. 2019)
Post Hospital Syndrome: Is Stress of Hospitalization Causing Harm? (Caraballo C et al. 2019)
Post-intensive Care Syndrome (Society of Critical Care Medicine)
Mental Health and Kidney Disease (American Kidney Foundation)
Depression and Kidney Disease (Kidney Care UK. org)
Work
Coping with Stress at Work (American Psychological Assoc.)
5 Ways to Wellness (Mind.org)
Mental Wellbeing: Self- Care & Relaxation
How Deep Breath Can Be Helpful for Mental Health (AU-NZ Mental Health Assoc)
9 Breathing Exercises to Relieve Anxiety (Very Well Mind.org)
EFT Tapping: A Scientific Guide on Emotional Freedom Technique (Everyday Health.com)
Meditation: A simple, fast way to reduce stress (Mayo Clinic)
3 Ways Meditation Can Help Your Heart, Body and Mind (Penn Medicine.org)
5 Ways to Well Being (Mind.org, under Workplace)
Guided Visualization: Dealing with Stress (video, NIMH
Breathing Exercises for Stress (NHS video: UK National Health Service)
Breathing Techniques for Stress Relief (Web Md)
Mental Health Benefits of Nature (NAMI ca.org)
Therapists – Types & Considerations
What Type of Therapist Do I Need (Two Chairs.com)
How do I know what type of therapy is best for me? (Mental Health Match.com)
Types of Talking Therapy (NHS, UK)
A Glossary of Therapy Approaches & Modalities (Mental Health Match.com)
7 Mental Health Treatments To Try If Talk Therapy Isn’t For You (Rodriguez-Cayro, Bustle.com)
Types of Mental Health Professionals (NAMI.org)
Different Types of Mental Health Treatment (Family Doctor.org)
(Material referenced in this article is neither endorsed nor recommended. As an overview, it does not provide complete information nor professional and verified content.
Contact your medical or mental health team for specialized and accurate information specific to your situation.)
About the Author: Linda LG Burke lives in Maine USA and volunteers with atypical HUS advocacy efforts through the aHUS Alliance Global Action team, and as a founding member of the int’l aHUS Community Advisory Board. Her professional background is in education (MsEd, BS Science & Math). As an aHUS family caregiver for two sons, Linda has contributed to aHUS efforts with international outreach and resource/content creation since 2009.

