FDA has approved the use of Iptacopan, brand name Fabhalta, for PNH.
Two trials demonstrated that this Factor B complement inhibitor worked for those transitioning from an existing complement inhibitor and also for treatment naive patients.
Iptacopan taken as a daily pill prevents the complement process which triggers the membrane attack complex from happening. In the case of PNH no “overnight” haemolysis of red blood cells results. In an earlier complement inhibitor some PNH patients were found to still need blood transfusions. Like Ravulizumab to some extent Iptacopan reduces the need for blood transfusions as there is less breakthrough haemolysis.
Nothing is known about the price of the drug, FDA does not concern itself with health economics. An interesting article just recently published about the potential price for the pill suggest it could be very little, if at all, cheaper than Ravulizumab because of the incremental quality of life years gained for a PNH patient. It would be more cost effective per QALY particularly as the cost of a transfusion nurse time is saved.
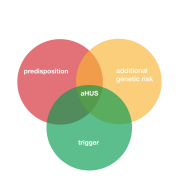
There are ongoing trials ( see aHUS Trial Watch 15 and 15 update. ) for use in treating aHUS patients and their success depends a lot on recruiting enough trialists. Although aHUS patients have not experienced the breakthrough haemolysis that PNH patients have, the incremental QALY would be less , there would be saving of the time spent on 6 or 7 infusions per year.
In the article a threshold monthly cost of $61k of treatment of PNH was computed assuming a willingness to pay $150k cost per QALY. Iptacopan could. be priced at 50% more than Ravulizumab and still be regarded as more cost effective. Lower willingness to pay affordability levels e.g. in UK £30k cost per QALY would require a lower price deal. A lower price still for aHUS treatment.
At those prices would it be affordable in countries that have no access to treatment at present? aHUS patients would need a price which not only shows “savings” not “costs” per QALY but at a price that a funder is willing to pay. Otherwise Iptacopan may not be the answer for many aHUS patients around the world.
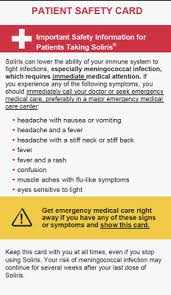
For Iptacopan the responsibility and burden on treatment would then fall to the patient each and every day day as the trough level of active ingredient drops quicker than a Ravulizumab dose. So daily treatment for some until treatment is not needed , and withdrawal is swifter.
Article No. 624