There have been moments and events in the past where someone whose endeavours make a significant difference for those who have been diagnosed with aHUS today. This is about one.
About someone who one day was inspired enough to name the disease that patients are now told they have. His name was Conrad Von Gasser. He died over 40 years ago but in 2015 someone who had met him and corresponded with him wrote this article for the first aHUS Awareness Day (which itself was an historic event!)
It was published on the 60th anniversary of the day the disease name appeared in public in a journal.
It is now a privilege for Global Action to publish Professor Bernard S Kaplan’s article about Von Gasser. and contemporaries, who changed the course of aHUS history when he wrote three words ( in German) on the death certificate of one his young patients, Baby Bodmer in the Children’s Hodpital in Zurich.
“Hamolytisch-uramiche Syndrom” or Hemolytic-Uremic Syndromes.
Day 6 to International aHUS Awareness Day ( part 1) – awareness of the history of aHUS
Bernard Kaplan (far right ) alongside Conrad Von Gasser
The cowbell belonged to Professor Conrad Von Gasser.
A tribute to Professor Conrad von Gasser [1912 – 1982] on the 60th anniversary of the first report of The Hemolytic Uremic Syndromes.
Bernard S. Kaplan, MB BCh, FAAP, Division of Pediatric Nephrology,The Children’s Hospital of Philadelphia, Professor of Pediatrics and Medicine,The Perelman School of Medicine at The University of Pennsylvania Philadelphia, PA 19066.
Gasser’s seminal paper entitled Hamolytisch-uramiche Syndrome [HUS] was published on September 20th 1955 [1]. In 1977 he had written to us requesting copies of our papers on HUS [this was before the days of the Internet]. I sent him reprints and invited him to visit the Montreal Children’s Hospital where, in 1978 [Fig 1], he gave a memorable lecture on his syndrome. Professor Gasser, a pediatric hematologist, was a gracious, thoughtful and generous man. He told us about his interest in the anemias and how he had begun to notice that some children with acute anemia had bizarre shaped erythrocytes. These fragmented red blood cells were called schistocytes. He and his co-worker, to whom he gave unstinting credit, selected five cases, which, in addition to evidence of hemolysis were severely ill with thrombocytopenia, acute renal failure and cerebral symptoms. All of the five patients died. Four had vomiting and diarrhea and one had pneumonia. Gasser believed, and continued to stress in his lecture as well as in a chapter in 1978, that the essential feature that distinguished HUS from Thrombotic Thrombocytopenia [TTP] was the severe renal involvement in the former, and the multi-organ involvement in the latter.
When I met Professor Gasser in 1978 he congratulated Keith Drummond [my Montreal mentor] and me for our editorial titled The hemolytic-uremic syndrome is a syndrome [2]. He gently chided us because he pointed out that his original paper was not entitled Hemolytic Uremic Syndrome but Hemolytic Uremic Syndromes. In German, he explained, syndrom is the singular for syndrome. However, he was generous in his praise for the fact that we had restated his concept.
Conrad von Gasser presented me with a Swiss cowbell [Fig 2] and asked me to ring it whenever the first International Symposium on HUS was to be held. In September 1982 I wrote to Prof. Gasser to inform him of my intention to dedicate the first symposium on HUS at an international conference to him. He died a month before my letter reached his office. And so, in Hannover, Germany, I rang the bell in his honor and in his memory in 1983 [3]. At The Hospital for Sick Children, Toronto, on September 9th 2015, I presented a lecture entitled Re-imagining the Hemolytic Uremic Syndrome at Grand Rounds and talked again about the cowbell.
Professor Gasser in his initial and subsequent publications gave a name to his syndrome, or as he stressed, syndromes. He and his colleagues differentiated HUS from TTP [although it took about 50 years for this to become accepted fully], described what we now recognize as S. pneumoniae HUS, and familial HUS, and recurrent HUS. Although many of their patients had diarrhea and vomiting Gasser et al did not recognize the diarrhea as a prodromal feature of HUS.
In 1992 we were honored when Professor E. Gautier and Professor R.E. Siebenmann contributed a chapter to our book Hemolytic Uremic Syndrome and Thrombotic Thrombocytopenic Purpura. As the co-authors of Gasser’s original paper they were in a unique position to describe The Birth of the Hemolytic Uremic Syndrome [4].
In regard to HUS, few came before Gasser but large numbers came after him. Joan Wagner, a South African pediatrician, while working at Great Ormond Street Children’s Hospital, may have been the first to report a case of HUS in an infant under the heading Acute Tubular Necrosis with Anemia [5]. There are now 6904 listings on HUS in PubMed. Madame Rene Habib made major contributions to our understanding of the pathology of HUS.
After Gasser et al. the second seminal contribution was Carlos Gianantonio’s description of the Diarrheal form of HUS [Fig 3]. His team advocated using early peritoneal dialysis and described the long-term histopathological outcomes of diarrheal HUS [6].
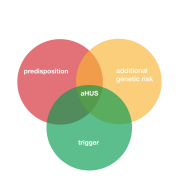
Barnard and Kibel, 1965, were the first to differentiate between typical and atypical HUS [7]. They noted that Diarrhoea of early onset was present in 10 of our 11 cases, and this has also been stressed in many others… but is not mentioned in the series by Gasser et al. Our atypical case, they noted, gave no history of diarrhoea. They also speculated in 1968 that HUS was caused by an E. coli infection [8]. Gervais et al, in 1971, used the term atypical [9] thereby predating that of Barratt et al’s classification of HUS into two groups – typical (epidemic, D+, diarrhea-associated) and atypical HUS (non-diarrhea associated, D- HUS) [10]. Neither group referred to Barnard and Kibel’s paper.
In 1978 we suggested that there was an inherited type of HUS that differed from an acquired type of HUS [11]. I subsequently drew attention to Hemolytic uremic syndrome with recurrent episodes: An important subset and I noted that these patients might have combinations of recurrent episodes and complement deficiency [12]. In 1992 I predicted that most all of these will [would] turn out to be genetic.
Several months after Gasser et al’s original paper McKay and Wahle reported a case of Epidemic gastroenteritis due to Escherichia coli O111 B4 [13]. This predated by 28 years the most important seminal contribution by Karmali et al [14]. Karmali et al. showed that E. coli 0157:H7 producing shiga toxin is the most important cause of HUS.
The third momentous discovery was the finding of mutations in the factor H gene that led to decreased concentrations of factor H in the alternative pathway of complement [15] and modestly noted that in light of these findings and previous reports of HUS in patients with factor H deficiency, we postulate that abnormalities of factor H may be involved in the etiology of HUS.
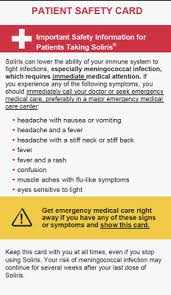
These abnormalities in the regulation of complement activity eventually led to a profound change in the treatment of atypical HUS with eculizumab [15].
References
- Gasser C, Gautier E, Steck A, Siebenmann RE, Oechslin R. [Hemolytic-uremic syndrome: bilateral necrosis of the renal cortex in acute acquired hemolytic anemia. Schweiz Med Wochenschr. 1955 Sep 20
- Kaplan, Chesney and Drummond Hemolytic uremic syndrome in families. N Engl J Med 1975.
- Kaplan, B.S., Bolande, R.P.: The Hemolytic Uremic Syndromes: The Dawn of a New Era. in Brodehl,J., Ehrich, J.J.H., (Eds.) Pediatric Nephrology, Springer–Verlag, Berlin, l984
- Gautier E, Siebenmann RE. The Birth of the hemolytic uremic syndrome. In. Hemolytic uremic syndrome and thrombocytopenic purpura. Eds Kaplan BS, Trompeter RS, Moake JL. Marcel Dekker, Inc. New York, 1992.
- Wagner J. Acute tubular necrosis with anaemia. Great Ormond St J.1954 Jun;7:66-72.
- Gianantonio CA, Vitacco M, Mendilaharzu F, Gallo GE, Sojo ET. The hemolytic-uremic syndrome. Nephron. 1973
- Barnard, Kibel . Haemolytic -uraemic syndrome of infancy and childhood. A report of eleven cases. Cent Afr J Med 1965
- KibelMA, Barnard PJ. The haemolytic-uraemic syndrome: a survey in Southern Africa. S Afr Med J. 1968
- GervaisM, Richardson JB, Chiu J, Drummond KN. Immunofluorescent and histologic findings in the hemolytic uremic syndrome. Pediatrics. 1971
- Fitzpatrick MM, Walters MD,Trompeter RS, Dillon MJ, Barratt TM. Atypical (non-diarrhea-associated) hemolytic-uremic syndrome in childhood. J Pediatr. 993
- Kaplan– Hemolytic uremic syndrome with recurrent episodes: An important s ubset. Clin Nephrol. 1977
- McKay DG, Wahle GH. Shwartzman phenomenon in fatal infantile diarrhoea due to Escherichia coli O-111, B4. Lancet. 1954
- Karmali MA, Steele BT, Petric M, Lim C. Sporadic cases of haemolytic-uraemic syndrome associated with faecal cytotoxin and cytotoxin-producing Escherichia coli in stools.Lancet. 1983
- WarwickerP, Goodship TH, Donne RL, Pirson Y, Nicholls A, Ward RM, Turnpenny P, Goodship JA. Genetic studies into inherited and sporadic hemolytic uremic syndrome. Kidney Int. 1998
- LegendreCM, Licht C, et al. Terminal complement inhibitor eculizumab in atypical hemolytic-uremic syndrome. N Engl J Med. 2013
Article No. 583