Can MedEd Encourage Specialists to Form TMA Teams?
Tiny clots which form in the body’s small blood vessels – in brief, that’s how thrombotic microangiopathy can damage vital organs such as the kidneys, brain or heart. Blood clotting (coagulation) occurs naturally to stop bleeding, but clots can also form unwanted barriers which restrict blood flow to cause negative impacts throughout the body.
Blood clots form when the lining of a blood vessel is damaged by a cut or otherwise injured, but there are risk factors and illnesses which can also trigger clot formation. Some factors involved in elevated risk for excess clotting include: inactivity due to an injury or long journey, some medications or cancers, pregnancy, and inherited blood clotting tendencies. Given the devastating effects of thrombotic microangiopathy, rapid diagnosis is key to effective treatment but that’s easier said than done.
Why aren’t there more “TMA Multi-Disciplinary Teams” commonly found in local hospitals and clinics? They do exist. But seldom do you see medical education or ‘Med Ed’ promoting this approach, which would be especially helpful to distinguish among underlying or causal factors. Treatment differs for syndromes which display characteristics of thrombotic microangiopathy some of which are: thrombotic thrombocytopenia purpura (TTP), disseminated intravascular coagulation (DIC), malignant hypertension (aka Hypertensive Emergency), antiphospholipid antibody syndrome (APS), and atypical hemolytic uremic syndrome (atypical HUS or aHUS). The diagnostic path seems more of a roundabout, with poor signposts that may lead to an incorrect conclusion or delay a correct diagnosis.
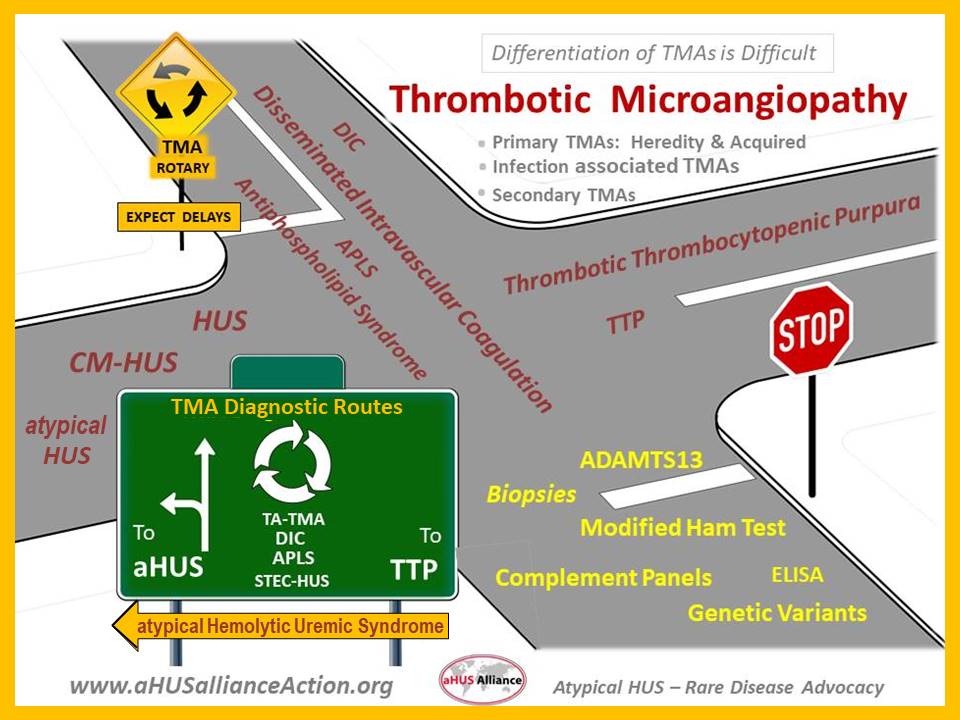
This dilemma of differentiating among TMAs has been reported in medical literature for well over 20 years, such as the 2004 Egan et al article on severe hypertension and considerations involved with diagnosis of thrombotic thrombocytopenia purpura (TTP). More recently, the pandemic has triggered a raft of scientific articles related to the effects of COVID-19 causing thrombotic microangiopathy with damage to the lungs, kidneys and heart. Given that infection can cause uncontrolled immune response in those people genetically predisposed to atypical HUS, it’s not surprising to see recent case studies noting atypical HUS triggered by COVID-19 or causing an aHUS relapse.
A multi-disciplinary approach to care to aid diagnosis and distinguish among types of thrombotic microangiopathy is often difficult in part because of wide variation in patient presentations and their clinical profiles. One thing is certain – with TMA one can expect a medically complex case and one where the clinical profile mimics several similar conditions. Anywhere that there’s blood flow, clot blockages in blood vessels can impact organ function and potentially may cause life-threatening events such as stroke or cardiac events. Infection may trigger an uncontrolled reaction of the part of the body’s immune system (complement), such as for SARS-CoV2 infection (COVID-19).
So why isn’t there a visibly strong and international movement among medical professionals to support creation of more “TMA Multi-Disciplinary Teams” in local hospitals and clinics? Think of the many advantages:
More accurate & rapid diagnosis yields better patient outcomes
Early differentiation of TMA type fosters increased potential for enrollment in clinical trials & research studies (particularly in regard to treatment-naive individuals)
Efficient & Effective: better asset allocation and Savings related to Cost and Time
Affords insights for medical students and residents, with a holistic approach to patient care
Promotes critical thinking for complex care cases, which can serve to broaden clinical experience/knowledge
Aids cross-specialty engagement and collaboration, expanding physician education within their medical institution and professional communities
Supports aspects of translational medicine, specifically ‘bench to bedside’ regarding use of new knowledge within clinical practice
Why is our aHUS-specific patient organization for such an ultra-rare disease commenting on the need for medical education and medical professional societies to promote a multidisciplinary team approach for TMA?
The aHUS Alliance Global Action team has long recognized aHUS as one condition among syndromes of thrombotic microangiopathy. Simply put – We live it. We experience delayed diagnosis. We visit multiple specialists. We endeavor to navigate complex care plans which are fragmented instead of rooted in a holistic approach.
The need for coordinated care to address the effects of thrombotic microangiopathy is great, and has only increased with the advent of COVID-related issues. Since 2017 the aHUS Alliance Global Action team has written articles on the need for multi-disciplinary care, and our patient organization initiated and hosted the Med Ed event Thrombotic Microangiopathy Symposium: through the Lens of aHUS. Our volunteers have developed a list of global aHUS & TMA study centers, as well as an international network of experienced and expert researcher/clinicians in the field of atypical HUS. If a small group of aHUS patients and family caregivers can do all this as volunteers, think what a team of researchers, clinicians and industry professionals might accomplish!
If you’ve developed a TMA interdisciplinary care team, that’s wonderful – and we invite you to share that information with other professionals to expand regions offering a TMA team approach. We commend those looking to create a multidisciplinary response to TMA cases within their practice or hospital, and suggest this article as a starting point Thrombotic Microangiopathy: A Multidisciplinary Team Approach (Gordon et al, 2017)
We hope that plenary sessions at conferences and symposia, academic and industry meetings, all include promotion of an interdisciplinary approach to thrombotic microangiopathy. The aHUS Alliance Global Action team forms connections and collaborates internationally in regard to multiple topics of high interest in the aHUS arena. Connect with us at: info@aHUSallianceAction.org
About aHUS & TMA
While only a handful of people per million have the rare disease atypical HUS, all are impacted by the devastating destruction caused by TMA. Symptoms of aHUS vary, but include hemolytic anemia (destruction of red blood cells), low platelets (consumed by clot formation), and organ damage due to tiny blood clot formation in capillaries and small arteries (thrombotic microangiopathy, TMA).
Patients with aHUS may experience wide-ranging issues with a variety of body systems and organs: kidneys, heart, lungs, peripheral & central nervous system, skin, eyes, and GI tract. According to one source (Scully et al, 2016), atypical HUS patients newly enrolled in the global aHUS registry experienced these types of issues within 6 months of disease onset: renal (75%), gastrointestinal (38%), cardiovascular (32%), central nervous system (25%), and pulmonary (19%). Clear indicators of strong need for a multidisciplinary approach to care for aHUS patients.
What’s in a Name, aHUS Terminology
Confusion regarding classification and nomenclature has become increasingly marked in recent years, to the point where the National Kidney Foundation has launched an international task force (click HERE FMI). The aHUS Alliance Global Action team’s website has multiple original articles on terminology regarding where complement and TMA intersects atypical HUS.
Not only is atypical HUS misdiagnosed as other, similar medical conditions it can be confused with regular HUS. This more common or ‘typical’ hemolytic-uremic syndrome (HUS) is sometimes known as Infection-associated Hemolytic Uremic Syndrome (IA-HUS) or may be named for the pathogen or cause for triggering HUS, such as E. coli–associated HUS (EHEC-HUS) or Streptococcus pneumoniae-associated hemolytic-uremic syndrome (SP-HUS).
In the future, complement-mediated TMA and associated terms will become clearer soon.
Additional Resources & Information
Thrombotic Microangiopathy & Precision Medicine
TMA Team Approach: Accelerating the Pathway to Diagnosis (video from TMA Boston (clinical, preceded by Patient Impact Statements) Event: Thrombotic Microangiopathy Symposium: through the Lens of aHUS
TMA Research, directly related to Atypical HUS Over 800 publications, see our TMA listing.

