When it comes to advocacy why say there is aHUS and there is also aHUSs?
The rare disease aHUS is described as the thrombotic microangiopathy triggered by uncontrolled complement activity which itself is triggered by one of numerous triggering conditions. This pure form of aHUS can be seen with the intersection of the three circles.
The Three Circles: Kidney Failure, TMA, and Uncontrolled Complement
- Kidney Failure: This is a broad category affecting many people. Kidney failure can result from numerous causes, such as diabetes, infections, or genetic disorders. Only a small subset of kidney failure cases involves TMA and/or complement issues. Re-envisaging the diagram in reality this circle is many times bigger than the other two.
- Thrombotic Microangiopathy (TMA): TMA is a process where small blood vessels become damaged, leading to blood clots, red blood cell destruction, and organ damage. TMA can occur with or without uncontrolled complement activation and may or may not affect the kidneys. This circle is much smaller than the kidney failure but in turn it is much larger than the uncontrolled complement circle.
- Uncontrolled Complement Activation: The complement system is part of the immune system. When it becomes overactive (uncontrolled), it can damage blood vessels and organs. This can happen with or without TMA and with or without kidney involvement and is a much smaller circle.
Where is aHUS?
“Pure aHUS” sits at the intersection of all three circles: it involves kidney failure caused by TMA, which is driven by uncontrolled complement activation. This is the core definition of aHUS. The area of the intersection is extremely small and may only be a circular dot “.” in relation to the other circles to reflect reality.
However, not all cases are so straightforward, and variations exist.
The interplay of these three conditions leads to different presentations of aHUS:
- Complement-Mediated TMA Without Kidney Damage: In some rare cases patients experience TMA caused by uncontrolled complement but without kidney injury. These cases don’t fit the “uremic” (kidney-related) part of aHUS, so they may not be classified as aHUS but as “aHUS-U” despite sharing similar mechanisms and challenge the traditional definition of aHUS. Still benefitting from the same treatment as Pure aHUS yet there is no answer why it can happen. Understanding the science behind what may be different could be beneficial to all.
- aHUS with Additional Organ Damage (aHUS+): Some aHUS patients experience damage to other organs (e.g., heart, brain, or lungs) alongside kidney failure. This could be called “aHUS+” to indicate the broader organ involvement, but it’s still rooted in complement-mediated TMA primarily affecting the kidneys.
So why are those who have the pure form of aHUS in the intersection? They were at risk and the likelihood of onset occurred.
aHUS is often linked to genetic mutations in the complement system, but the story is more complex:
- Triggers Alone: all people can experience one or more of “triggers” (like infections or stress) at some time in their lives and it could theoretically start complement overactivation, but it doesn’t because their complement is controlled the way nature intended.
- Genetic Mutations : Some patients have rare genetic mutations that predispose them to uncontrolled complement activation. These mutations, combined with a “trigger” (e.g., infection, pregnancy, transplant or stress), can initiate TMA and lead to aHUS or aHUSplusG However, not all people with these mutations develop aHUS, they may remain lifelong aHUS carriers. Other factors (like common genetic variations or protective mechanisms) may prevent it happening to them.
- No Genetic Mutations : In some cases, aHUS occurs without identifiable complement mutations. Something else—such as an autoimmune issue, medication, or an as yet unknown factor—disrupts complement control, leading to TMA and kidney failure. These patients may still receive an aHUS diagnosis but are aHUSminusG and benefit from complement-inhibiting treatments, but their underlying cause and prognosis may differ.
Simplifying the Diagnosis
So, who has “pure aHUS” or its variations? Here’s a breakdown:
- Pure aHUS: Kidney failure + TMA + uncontrolled complement activation. This is the classic form.
- aHUS+: Pure aHUS with additional organ damage.
- aHUS-U: Complement-mediated TMA without kidney damage, which may or may not be classified as aHUS.
- aHUSplusG: aHUS with identified complement mutations.
- aHUSminusG: aHUS without identified complement mutations, possibly caused by other factors.
Why does it matter?
Understanding these distinctions is crucial because they affect diagnosis, treatment, and prognosis. For example:
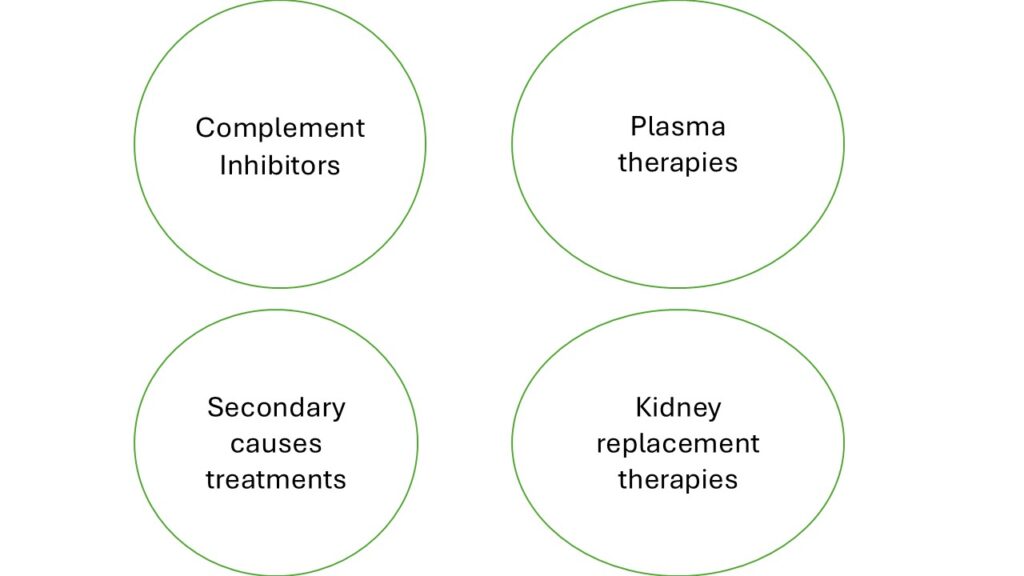
- Patients with pure aHUS or aHUS+ typically receive complement inhibitors (like eculizumab/ravulizumab) to stop the damage done by their complement system until a TMA response ceases and he kidneys and other organs are protected and can recover.
- Those with aHUSminusG may need additional treatments to address underlying non-genetic causes.
- Patients with complement-mediated TMA but no kidney damage aHUS-U may not fit the aHUS label so difficult to diagnose but could would still benefit from similar therapies .
Final Thoughts
aHUS is not a one-size-fits-all diagnosis because of the interplay of the factors in the six circles above. It’s a specific condition defined by kidney failure, TMA, and uncontrolled complement, but variations exist based on genetics, organ involvement, and triggers. By separating the “circles” of kidney failure, TMA, and complement activation, we can better understand who has aHUS, who might have a related condition, and how to tailor treatment. If you’re an aHUS patient, your experience—whether it’s pure aHUS, aHUS+, or another variation—helps shape your unique diagnosis and care plan.
Advocacy for aHUS patients has its limitation in capacity and capability. It cannot be for all kidney disease , all TMAs or all complement. Neither it should be. There are many other organisations to do most of that. How much is left is a key decision going forward as the disease aHUS is divided up into bits which may need their own advocacy.
Now where do these treatments work and overlap?
Article No. 738


