So aHUS is a genetic disease caused by the aHUS gene.
Many people talk about “the aHUS gene” as though it was something that gives some people aHUS.
There is no such thing.
Individual patients who have encountered aHUS are now seen in an entirely different way best described by this diagram below.
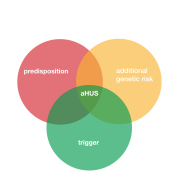
Each aHUS patient has become such because of a very small genetic differences which make them predisposed to aHUS , but which are also putting them at different risks of getting aHUS when one of many triggering hits breaks through. It puts them at the centre of the three circles.*
But turning it another way around aHUS is not inevitable. Those predisposed may have other genetic differences that put them at less risk ,or , may even protect them even though they may experience many of the same triggering hits as those who onset.
OK but aHUS is a Renal Disease though .
Yes aHUS is a renal disease; that is reflected in part of its name “uraemic” ; uraemia is raised level urea in the blood and results from loss of kidney function. However something also happens in the blood as the other part of the name “haemolytic” reflects red blood cells loss causing anaemia.
But these are symptoms but not how the disease operates within the body.
Operates?
The genetic differences in aHUS patients set up the conditions for a perfect storm of damaging activity in the blood. The storm, which itself is not felt by the aHUS patient, is known as thrombotic microangiopathy or TMA. The resulting clotting and destruction of red blood cells in the aHUS patient hits a critical point that symptoms are felt/seen in several of the patients’ organs, but particularly the kidney, hence its close association with it.
What feeds that storm is the aHUS patients own Complement System which is where their genetic differences lay.
The aHUS patient is at the centre of the second three circle diagram below
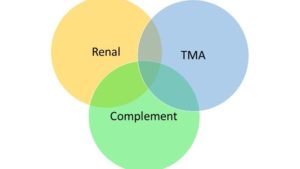
But again turning it the other way around and there are other TMAs without renal involvement but resulting from a complement genetic difference , as well as those with renal disease caused by TMA but with no Complement link .
Should those falling within those groups be regarded as aHUS patients, because some are at the moment.
So aHUS is just a subset of a much wider world of Renal , Complement and TMA diseases
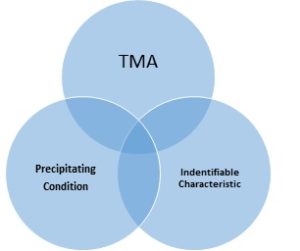
Indeed which leads us to look at aHUS from another perspective as just one kind of TMA where the precipitating conditions as seen in the first set of circles above result in disease characteristics which match with the symptoms of aHUS.
Again the aHUS patient is at the centre of a 3 circle diagram but surrounded by many other disorders in which the storm of TMA is due to other precipitating conditions, which result in illness characteristics which are not like aHUS though many are shared.
It’s a more chaotic world from which aHUS has to be discovered.
That makes things less clear cut then.
That is right but it does lead to a different way of thinking about aHUS , seeing it as just one part of a spectrum of TMAs as seen in the diagram of four circles.

aHUS is renamed as Complement HUS and has overlap links with STEC , or e coli (typical ) HUS with which it shares a name, and Secondary TMAs , where Complement plays a part, but the primary illness or condition defines those patients’ illnesses.
At one time all these were known as TTP (thrombotic thrombocytopenic purpura ) so you can see how thinking has changed over the past seven decades.
Seven decades?
Yes it was not until 1952 that TMA got its name, and then in 1955 HUS was first described.
OK so now I am now thinking
- aHUS is not the result of a single aHUS gene there are lots
- aHUS is not inevitable in those at risk
- aHUS is not just a Kidney disease
- aHUS is a rare clotting disorder
- aHUS is one of many thrombotic microangiopathies (TMA)
- aHUS overlaps with e .coli and other precipitating conditions within a spectrum of TMAs
That is right and thanks for thinking about aHUS today.
*Here is an example of aHUS where the three factors come together in an unusual way….
It is extremely difficult to predict whether an individual will present with aHUS ,even though from genetic testing, or probable familial susceptibility, an individual would seem predisposed to aHUS. This is because of the additional need for a trigger, as well as another genetic modifying factor.
The need for this triad of events to occur to bring on an episode of aHUS is very well illustrated in a clinical article “Postpartum aHUS Secondary to a Genetic Abnormality in Factor H Acquired Through Liver Transplantation” which can be read by clicking here.
The case involves a female who was not genetically predisposed to aHUS until she received a liver transplant. The donated liver came with a Complement Factor H ( CFH) mutation. All was well for five years until the patient became pregnant ; and after giving birth an episode of aHUS begun which resulted in end stage renal failure.
Further genetic tests showed that the patient also had a common CD46(MCP) genetic mutation in her kidneys which was the probable cause of the pregnancy becoming a triggering event.
The probabilities of having all the factors in the wrong place in the wrong time are very small.
As far as the documented incident is concerned the recipient’s aHUS experience is sporadic, and so the family are not at risk, but the family of the deceased donor may well still be.
Delve Deeper: Atypical HUS Clinical Channel on YouTube
Note: Featured image comes from aHUS Source

